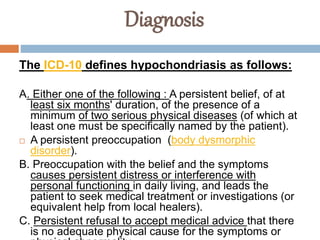
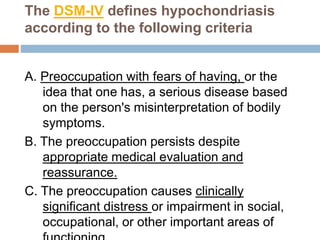
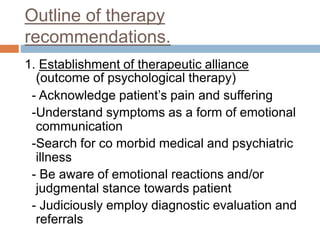
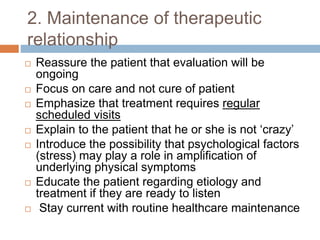
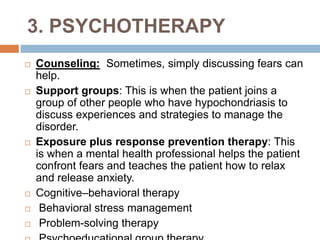
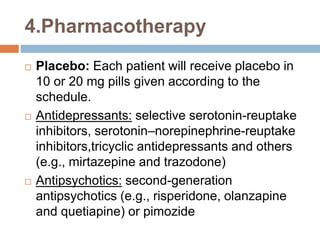
Hypochondriasis is characterized by excessive worry about having a serious illness despite medical reassurance. It involves misinterpreting normal bodily functions as signs of illness. The document defines hypochondriasis and outlines its features, symptoms, causes, diagnosis, and treatment approaches. Treatment typically involves establishing trust with the patient, ongoing reassurance, psychotherapy like CBT to address cognitive distortions, pharmacotherapy with antidepressants or antipsychotics, and lifestyle management.