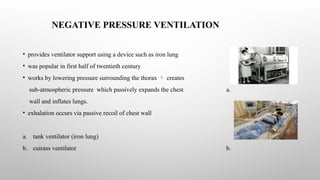
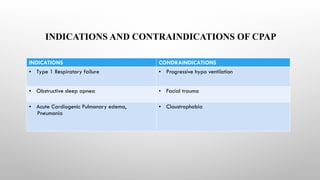
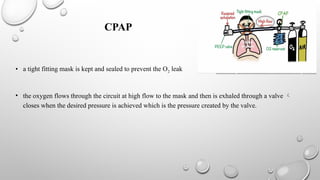
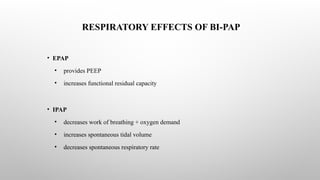
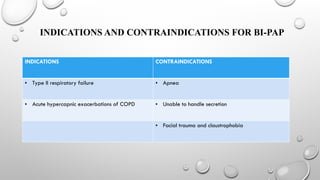
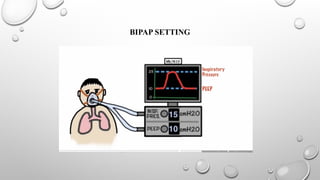
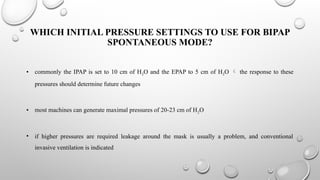
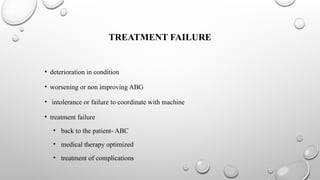
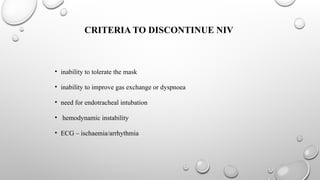
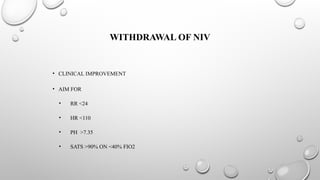
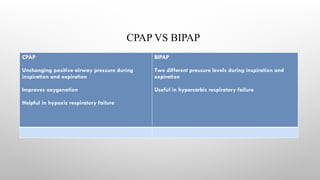
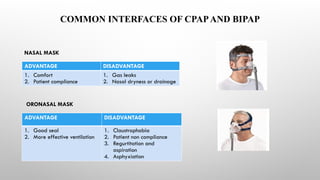
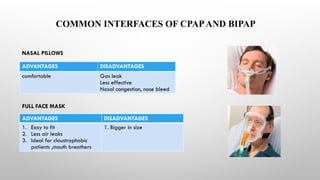
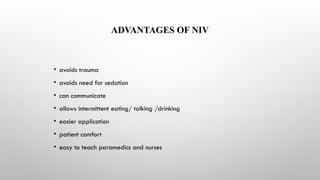
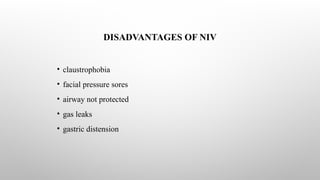
The document provides an overview of non-invasive ventilation (NIV), detailing its types, including negative and positive pressure ventilation methods like CPAP and BiPAP. It discusses the indications, contraindications, and advantages and disadvantages of each method, as well as monitoring patient responses and criteria for treatment failure. Additionally, it highlights common interfaces used in NIV and offers guidance on patient management and documentation.