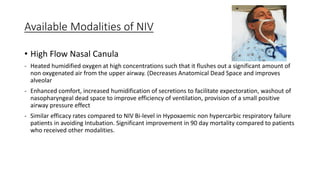
This document discusses non-invasive ventilation (NIV) for respiratory failure. It describes the types and causes of respiratory failure and lists selection criteria for NIV such as respiratory distress, abnormal blood gases, and respiratory acidosis. The benefits of NIV are reducing mechanical ventilation needs, ICU stay, and mortality. Goals of NIV are to reduce work of breathing, improve blood gases, and avoid intubation. Contraindications include poor mental status and hemodynamic instability. Modalities include high flow nasal cannula, bi-level positive airway pressure, and continuous positive airway pressure. Settings are titrated based on blood gases and comfort. Monitoring includes vital signs and blood gases to assess response.