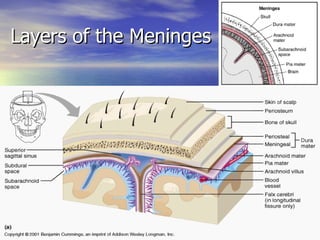
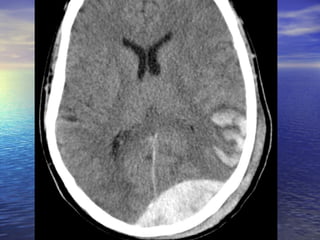
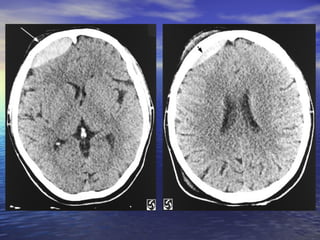
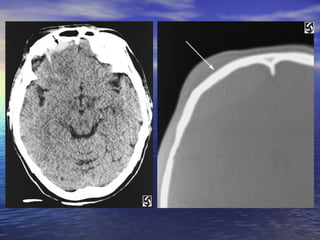
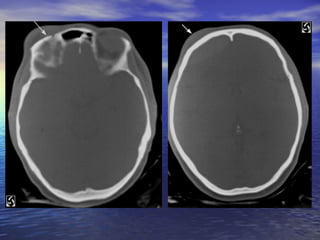
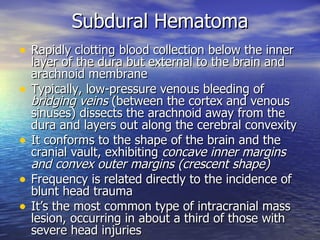
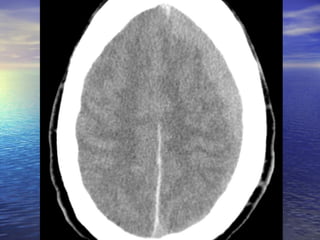
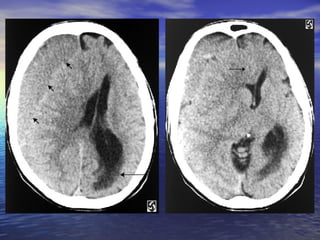
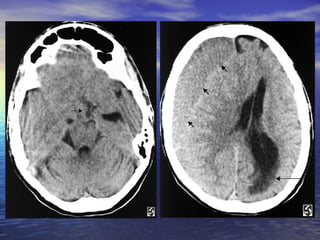
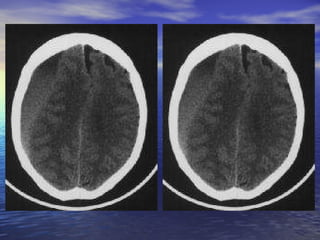
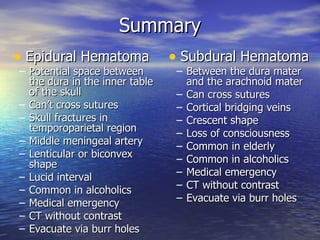
Epidural hematoma results from skull fractures that cause bleeding between the dura and skull. It presents as a lenticular or biconvex mass that cannot cross suture lines. Subdural hematoma occurs between the dura and arachnoid membranes from cortical vein tears. It appears as a crescent-shaped mass that can cross sutures. Both require urgent CT imaging and surgical evacuation via burr holes.