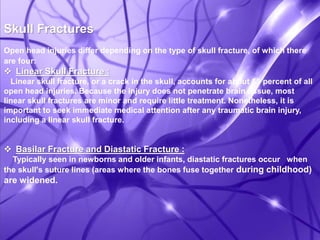
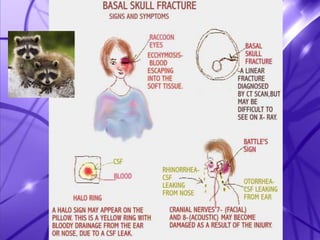
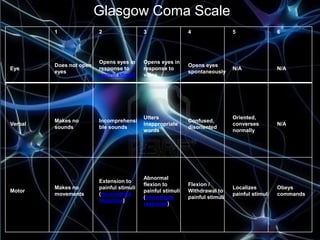
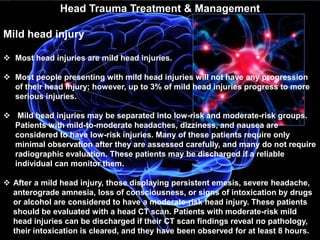
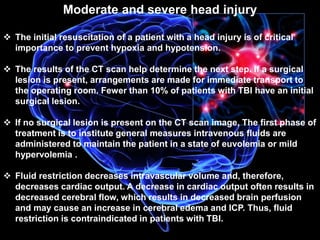
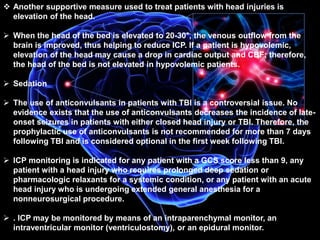
This document discusses traumatic brain injuries (TBI), including closed and open head injuries. It provides details on the causes, symptoms, treatments, and scales used to measure the severity of TBIs. The leading causes of TBIs worldwide are traffic accidents and falls. Closed head injuries account for about 75% of brain injuries and can range from mild concussions to severe injuries involving brain damage. Open head injuries involve skull fractures and have risks of infection, bleeding in the brain, and other complications if not promptly treated.