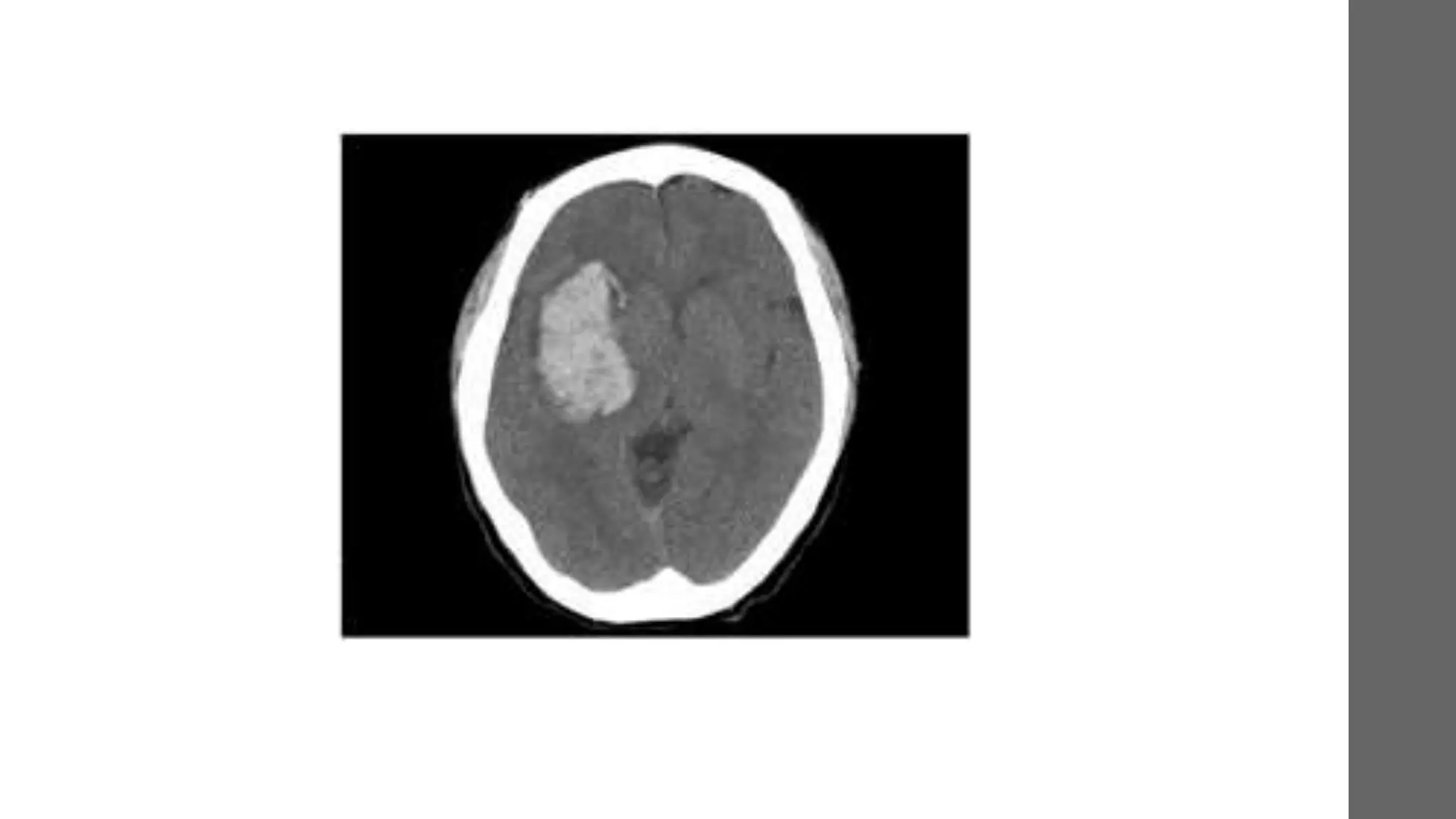
The document provides a comprehensive overview of intracranial bleeding, detailing types such as epidural, subdural, subarachnoid, intracerebral, and intraventricular hemorrhages, along with their respective causes, clinical presentations, and management strategies. It emphasizes the importance of neurologic assessment, appropriate diagnostic procedures like CT scans, and surgical versus non-surgical treatment options based on specific clinical scenarios. The document also highlights risk factors, epidemiology, and the mechanics behind each type of hemorrhage.