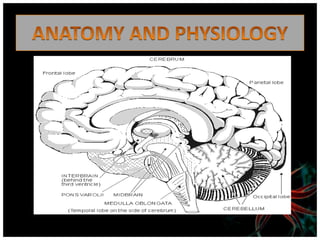
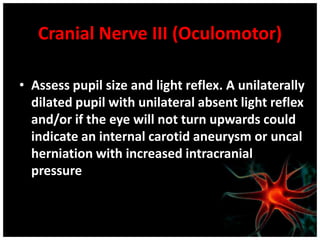
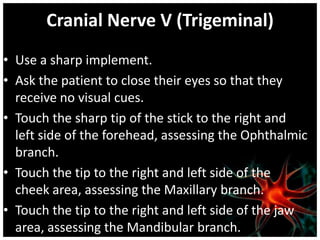
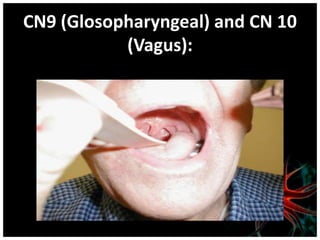
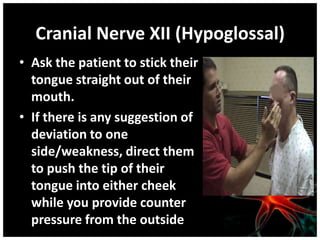
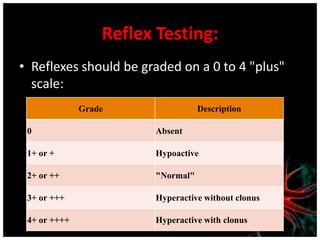
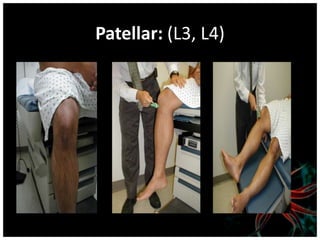
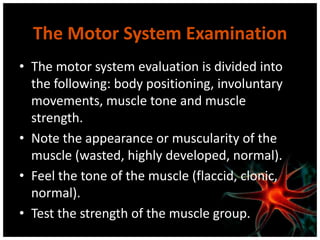
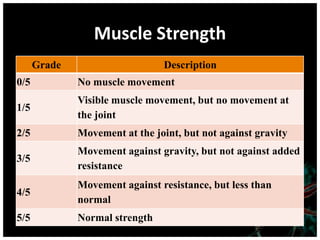
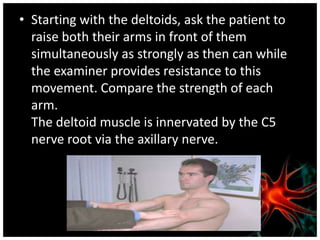
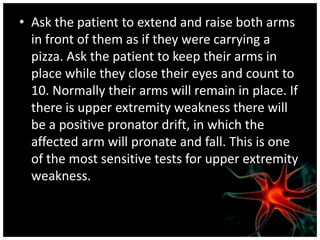
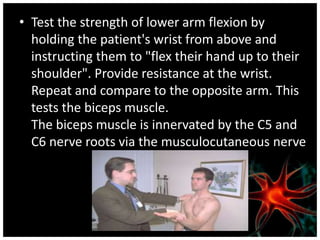
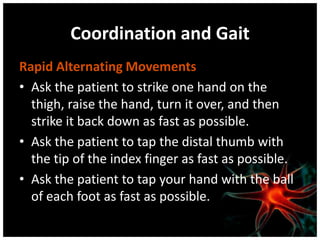
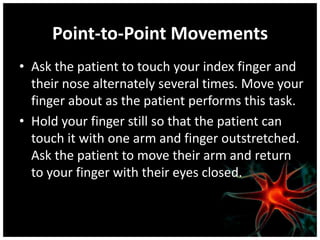
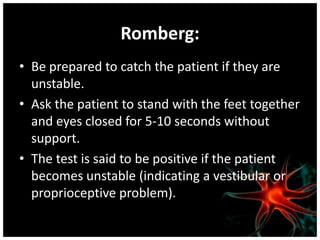
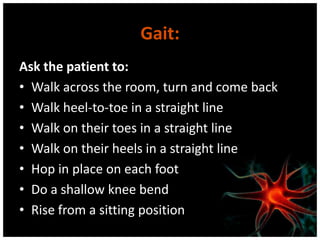
The document provides guidance on performing a neurological assessment to identify abnormalities. The assessment involves gathering information on symptoms, medical history, and conducting a mental status exam, cranial nerve assessment, reflex testing, motor and sensory exams, and evaluating coordination and gait. The goal is to screen for neurological disorders and determine the location and components affected. The assessment uses basic equipment and involves systematically testing various reflexes, sensations, strengths, and movements.