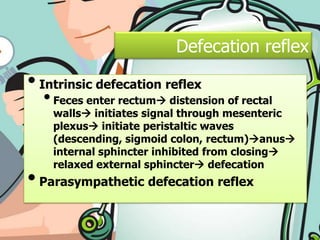
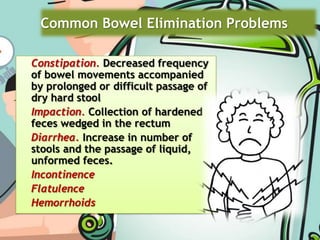
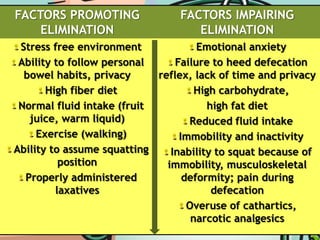
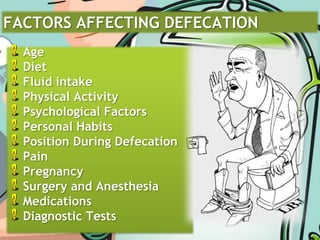
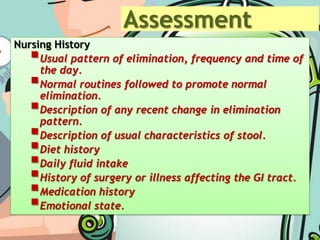
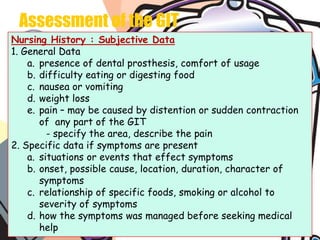
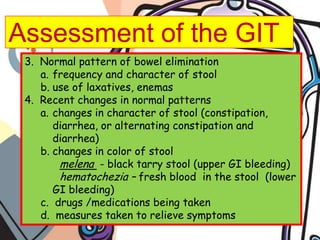
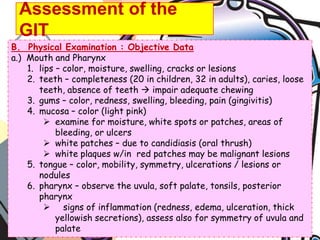
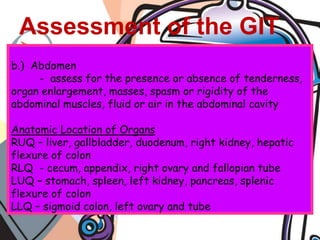
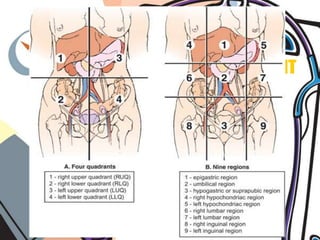
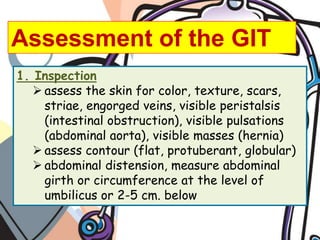
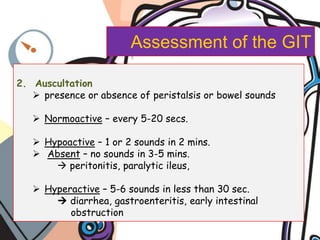
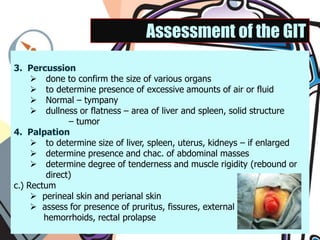
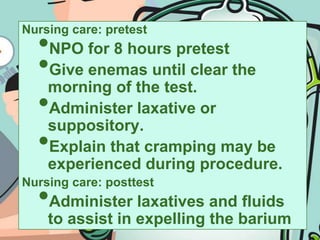
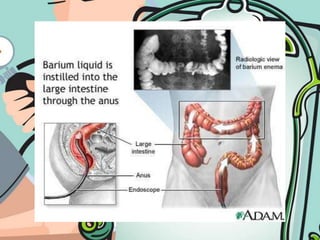
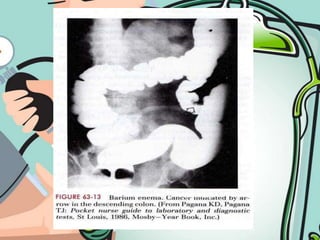
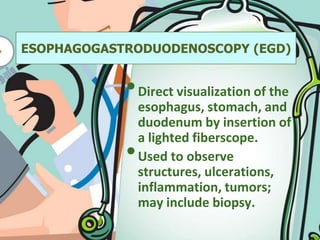
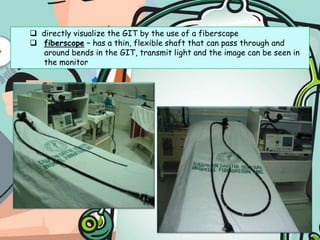
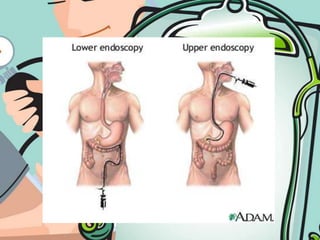
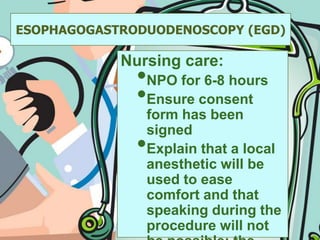
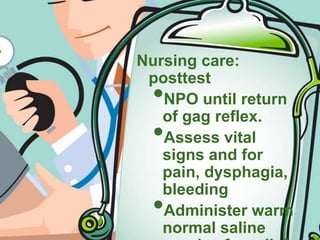
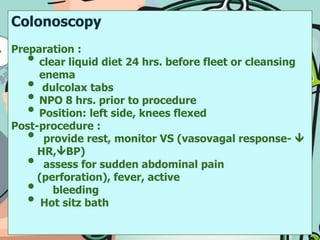
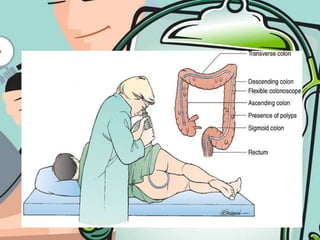
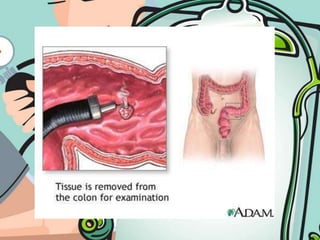
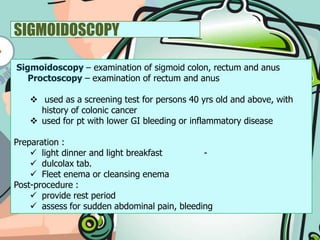
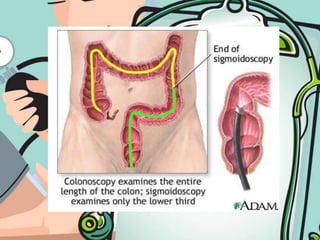
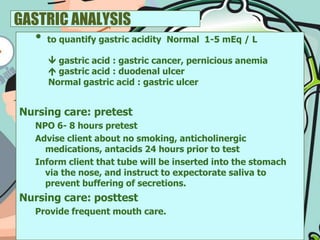
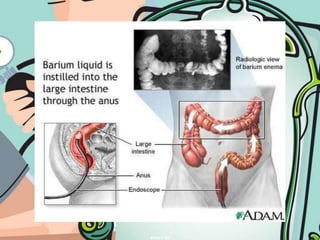
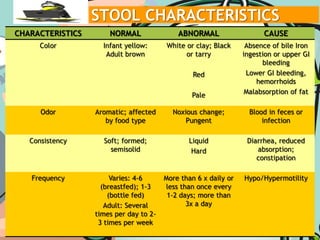
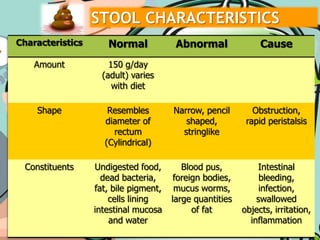
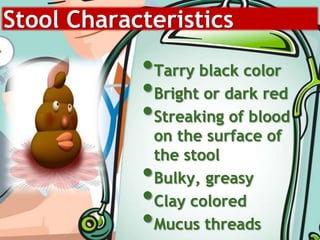
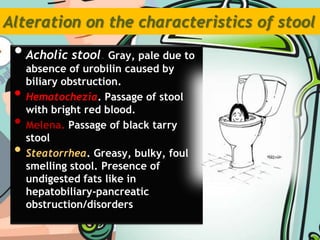
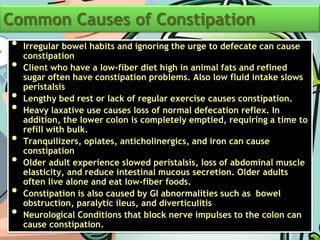
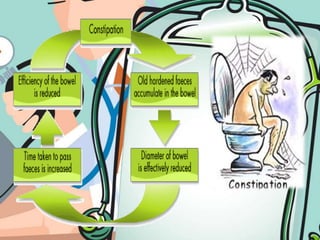
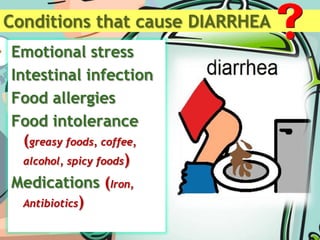
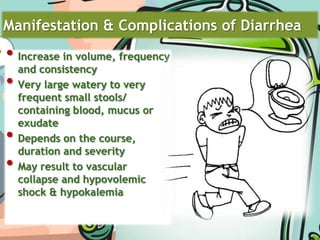
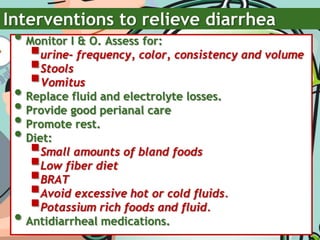
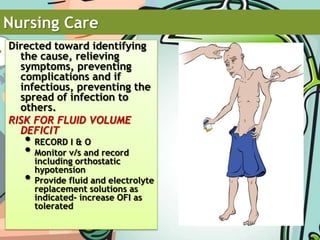
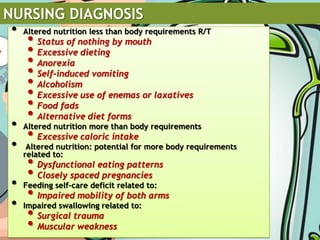
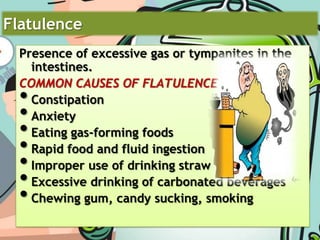
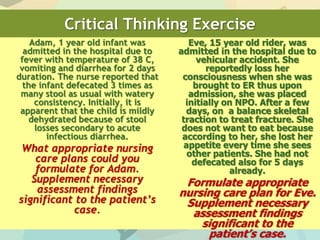
This document discusses defecation and common bowel problems. It defines defecation as the expulsion of feces from the anus and rectum, and describes the intrinsic and parasympathetic defecation reflexes. Common bowel problems mentioned include constipation, impaction, diarrhea, and incontinence. Factors that can affect defecation are also listed such as age, diet, fluid intake, medications, and psychological factors. The document provides details on assessing the gastrointestinal system through nursing history and physical examination. It concludes by describing various gastrointestinal tests and procedures.