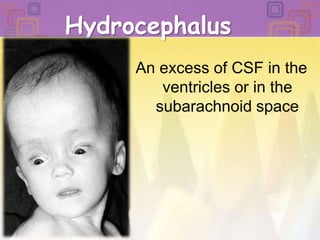
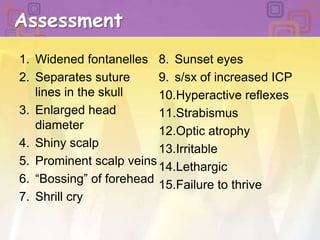
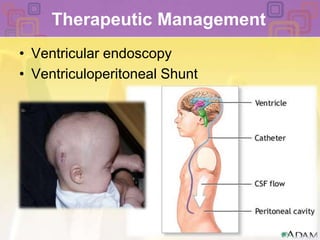
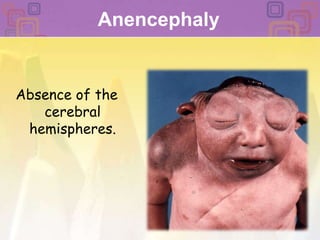
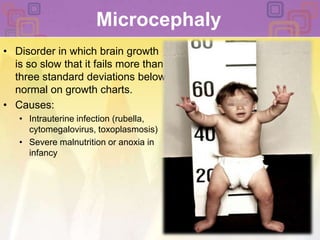
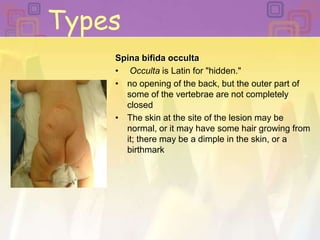
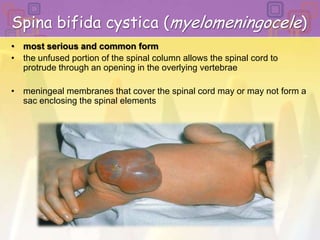
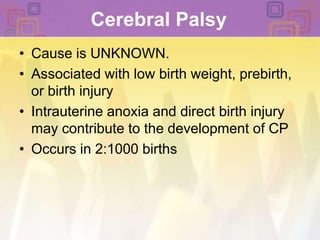
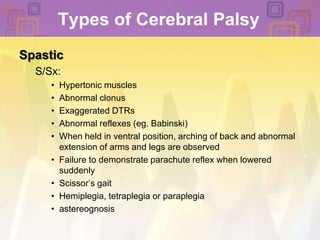
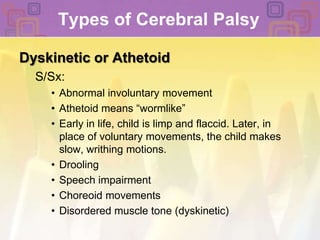
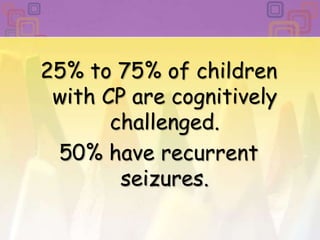
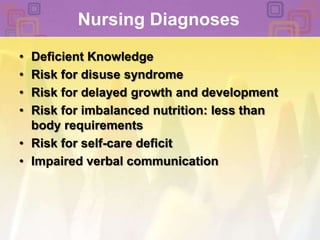
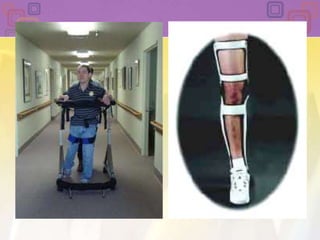
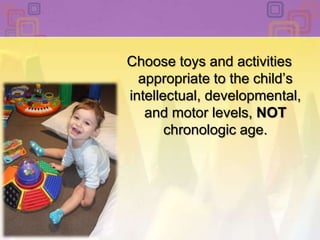
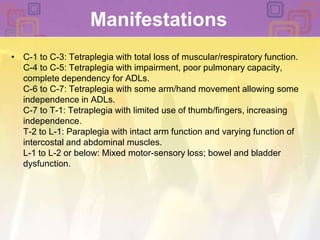
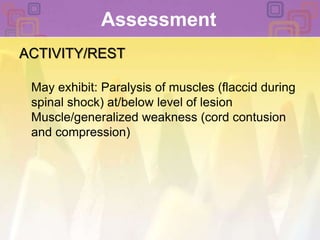
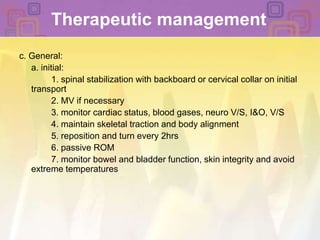
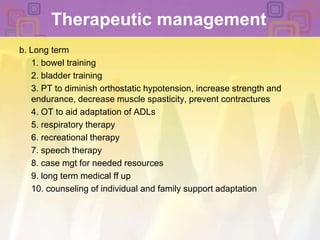
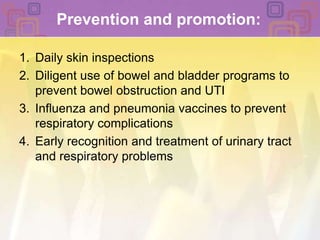
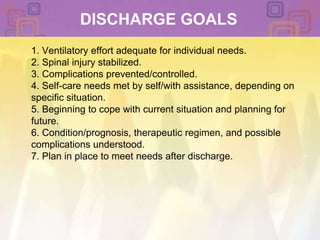
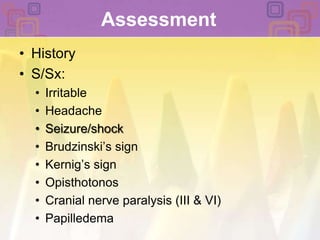
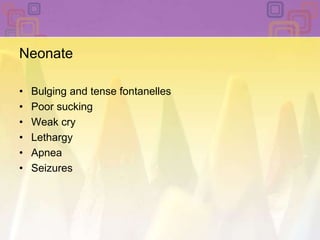
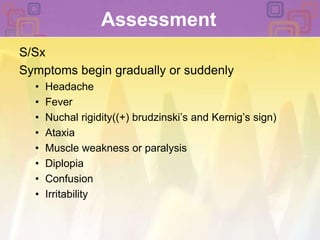
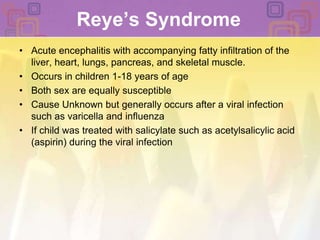
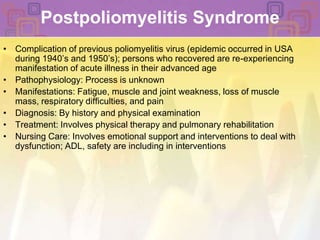
This document summarizes several pediatric neurologic disorders including hydrocephalus, neural tube defects, cerebral palsy, spinal cord injury, and infections of the central nervous system. It describes the causes, signs and symptoms, diagnostic tests, nursing diagnoses, and treatment approaches for each condition. Nursing priorities for patients include maximizing respiratory function, preventing further injury, promoting mobility, preventing complications, and supporting psychological adjustment.