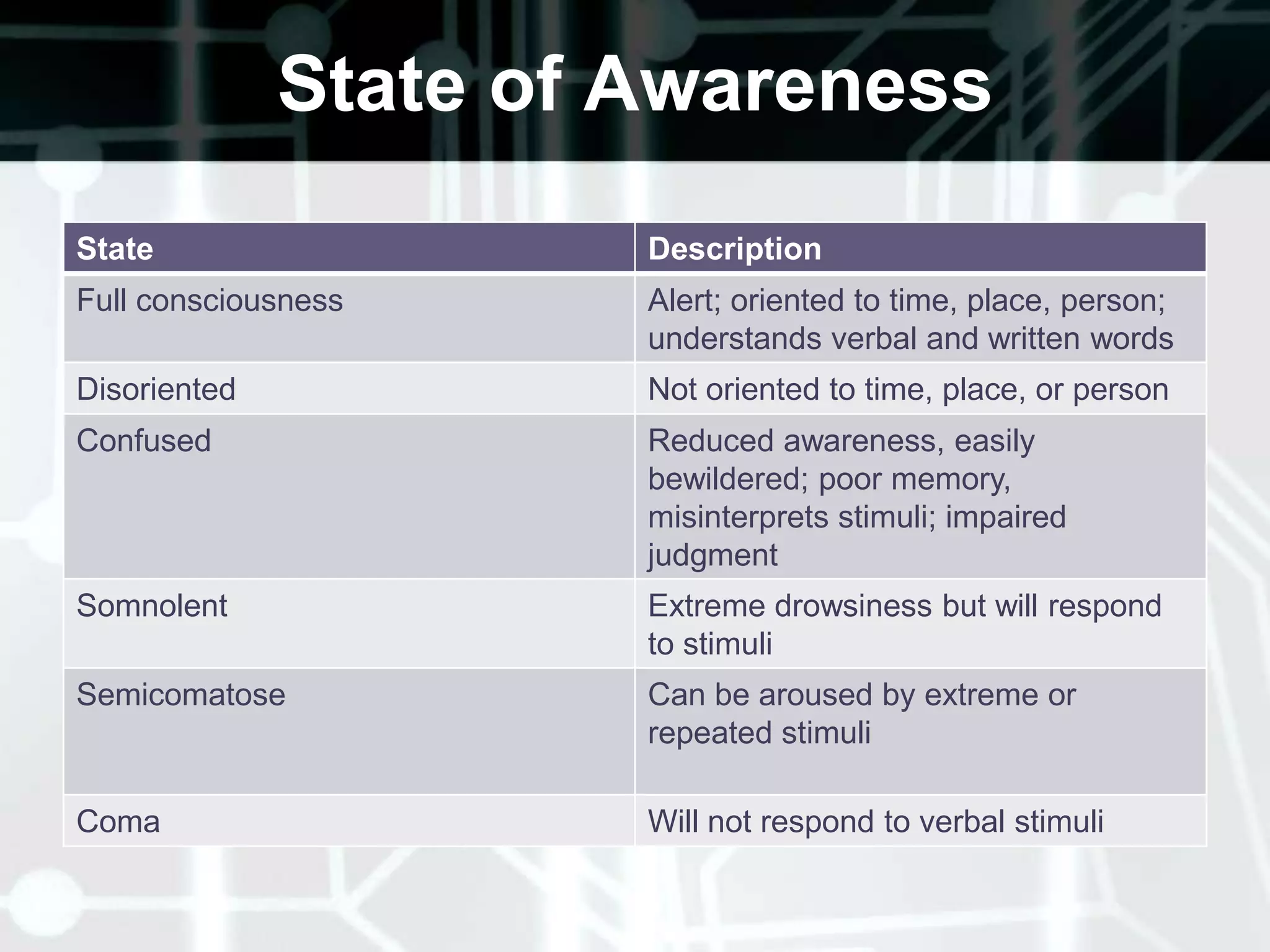
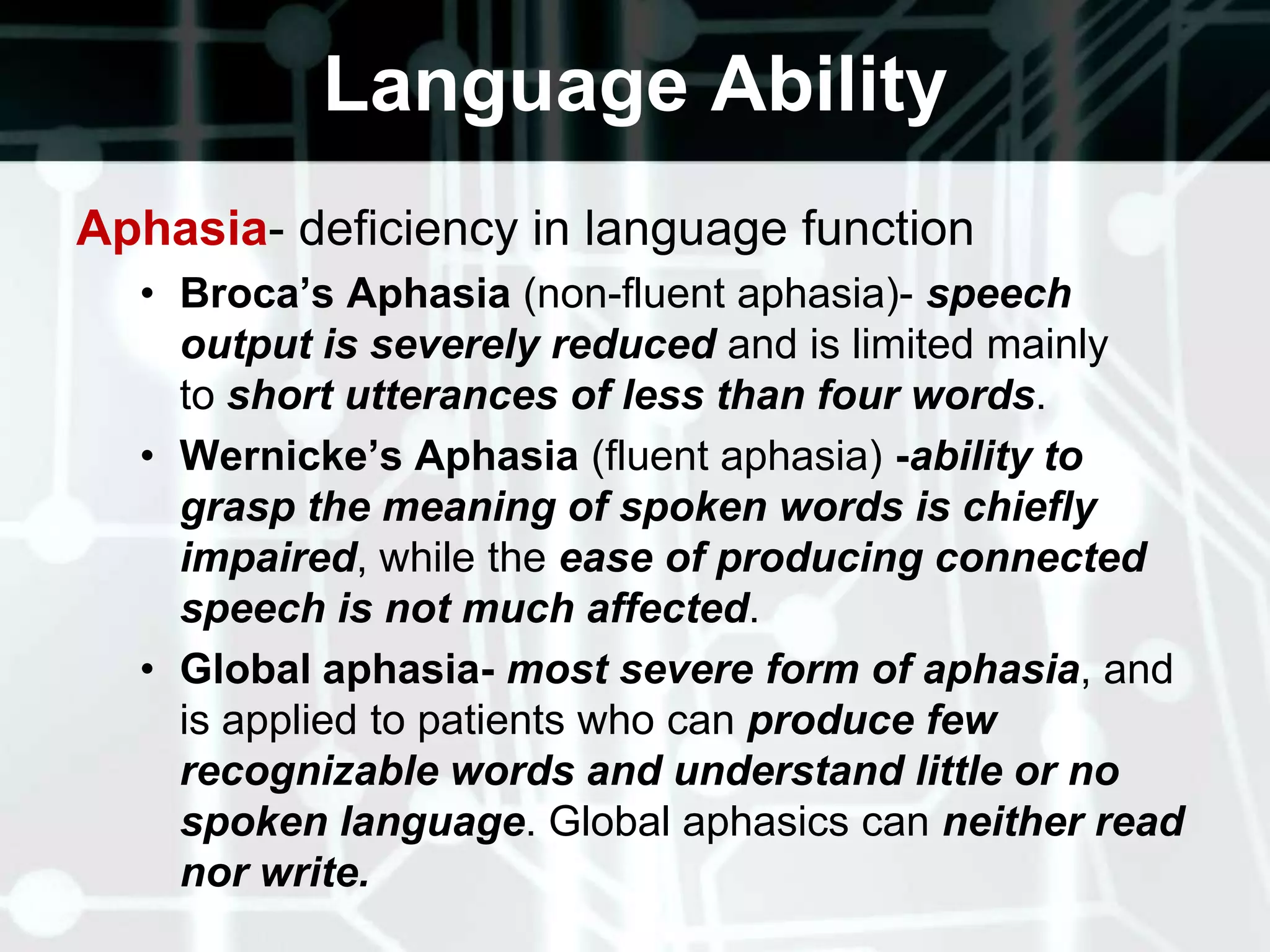
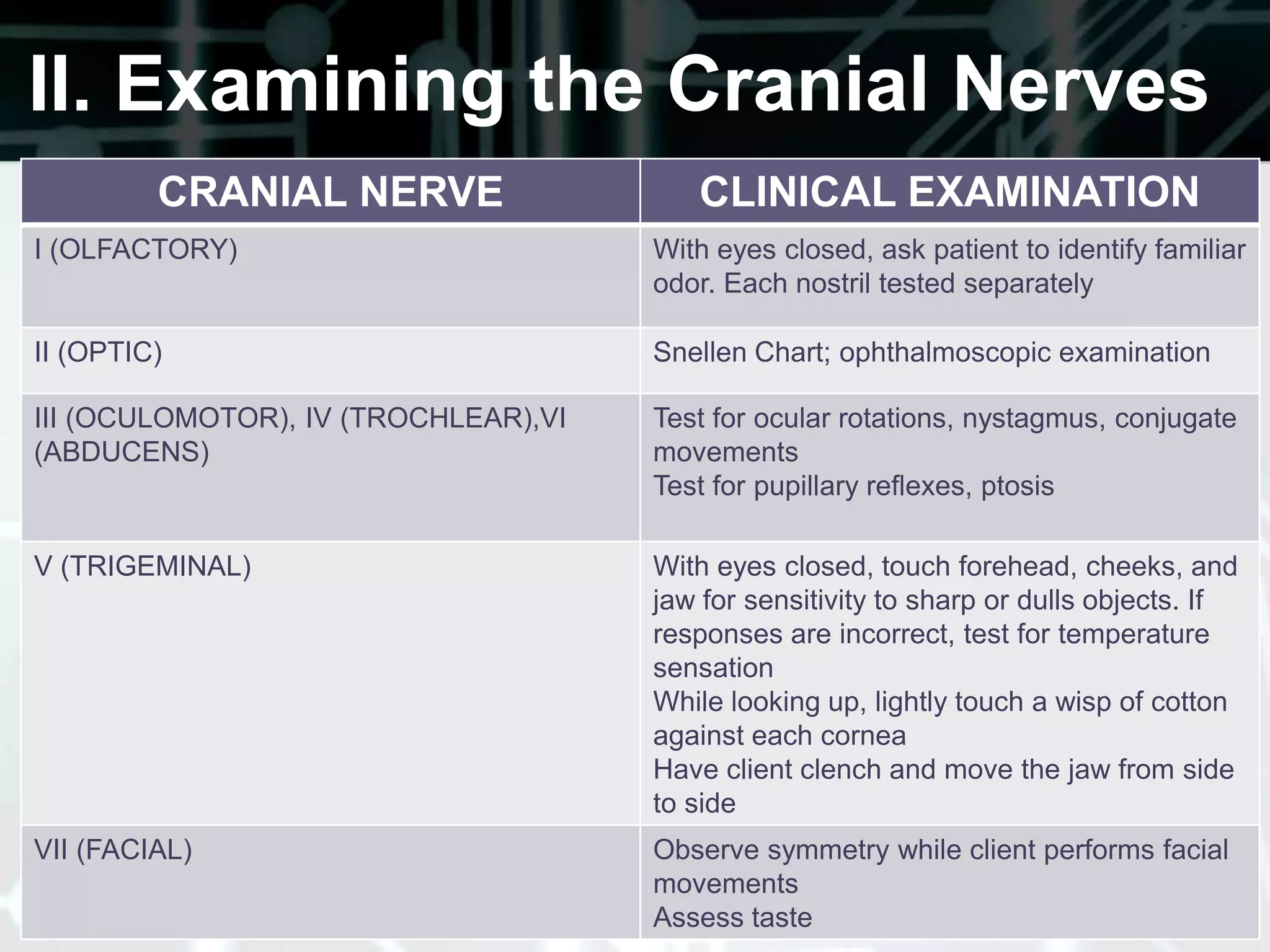
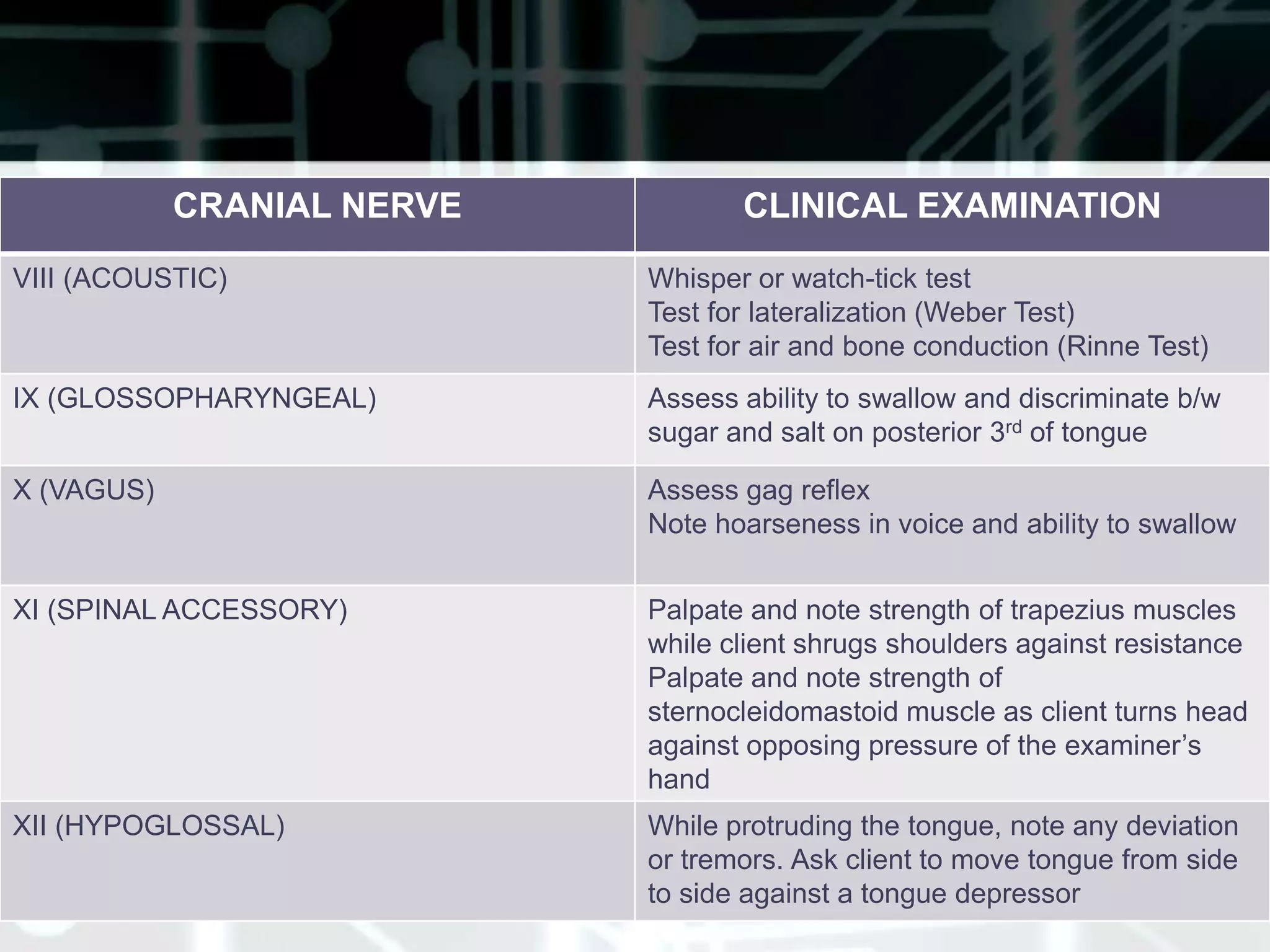
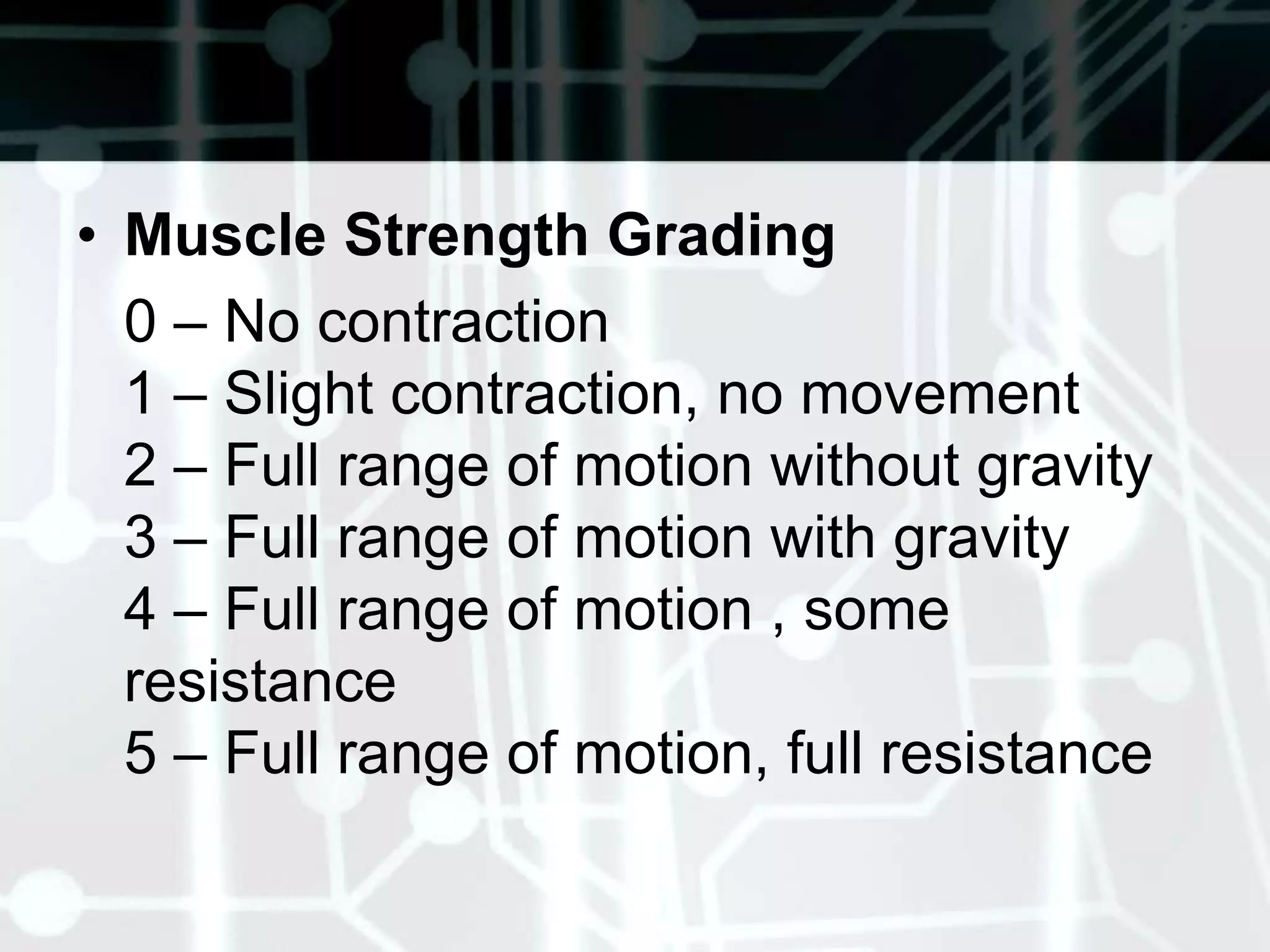
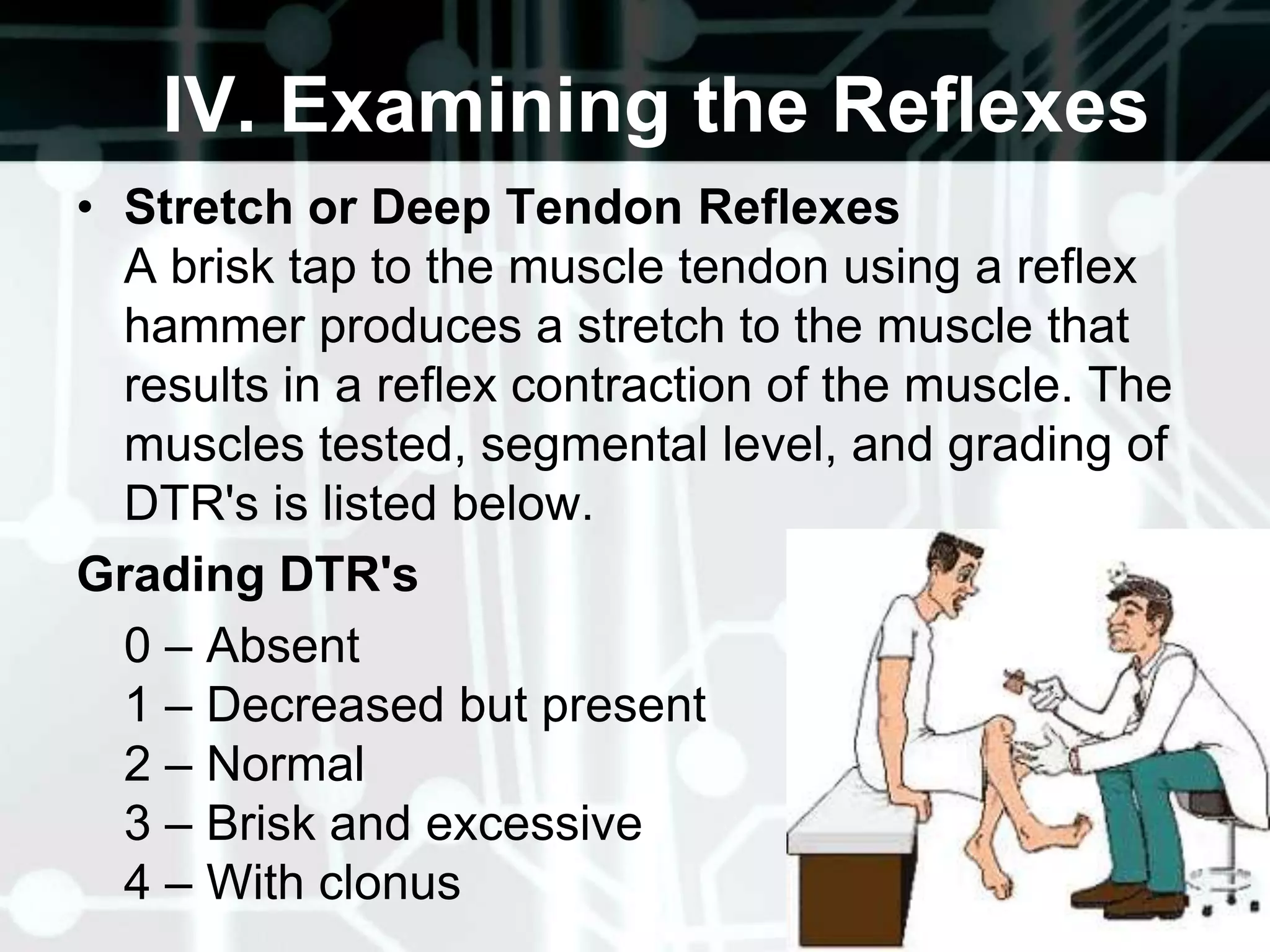
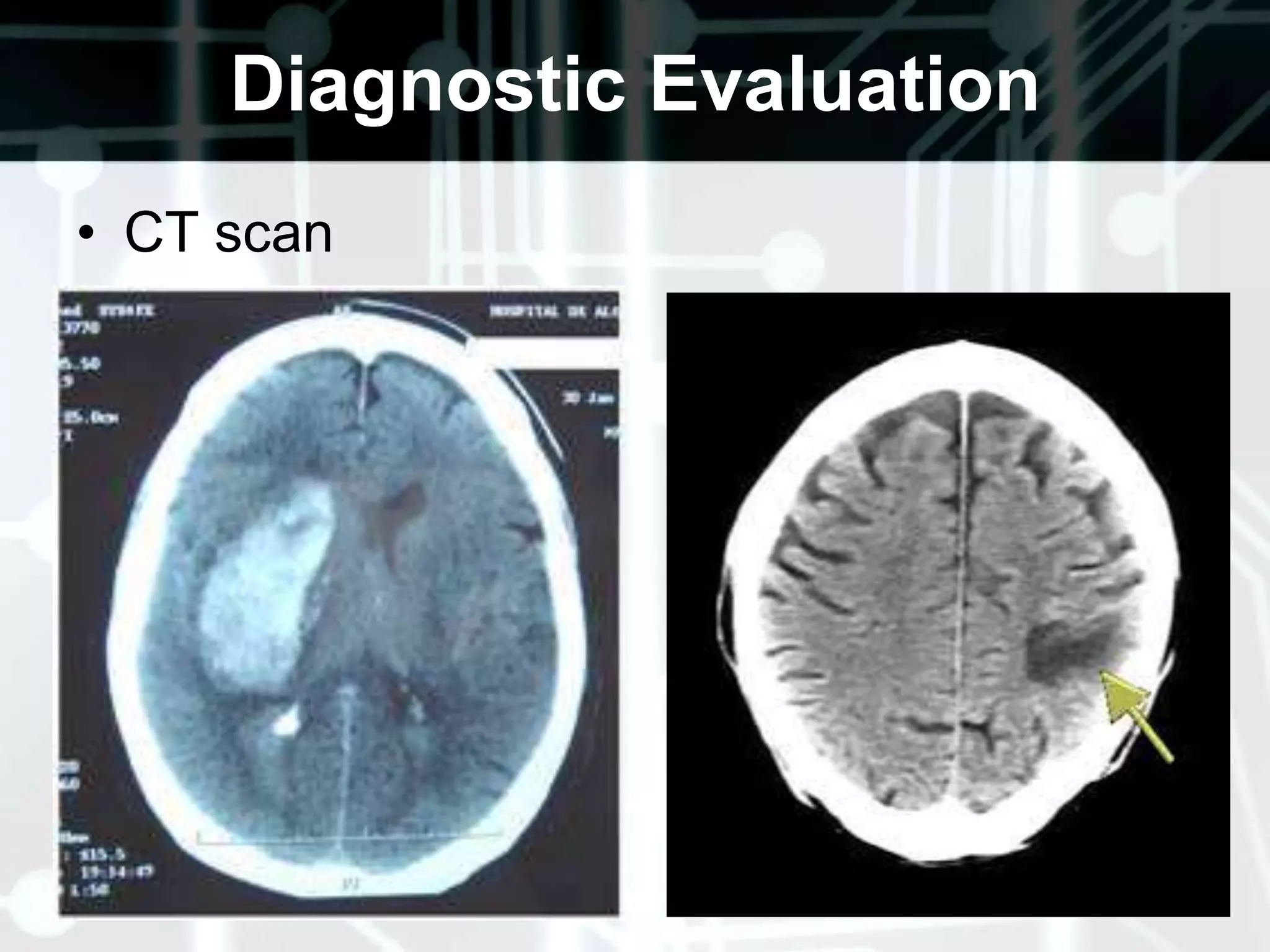
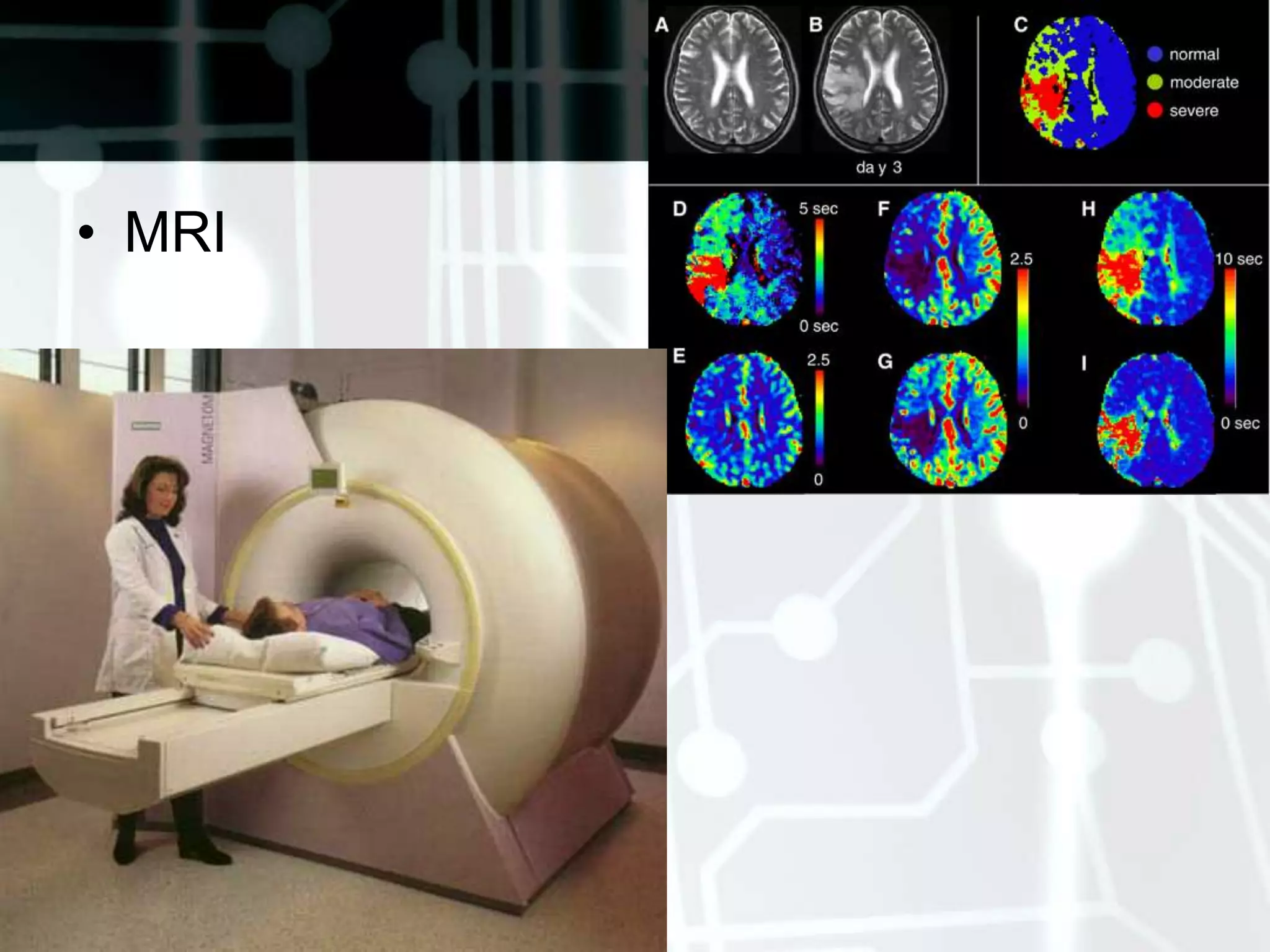
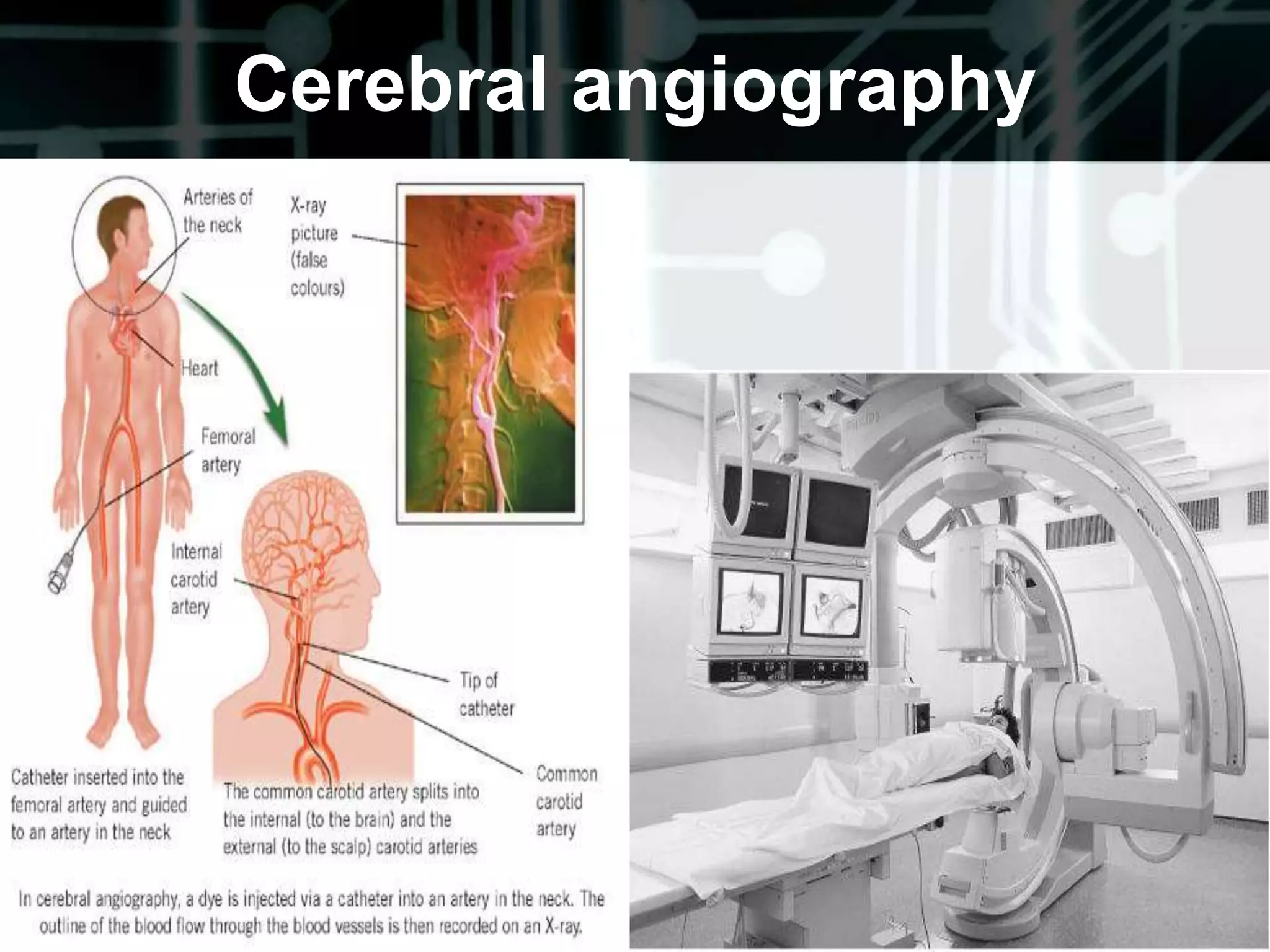
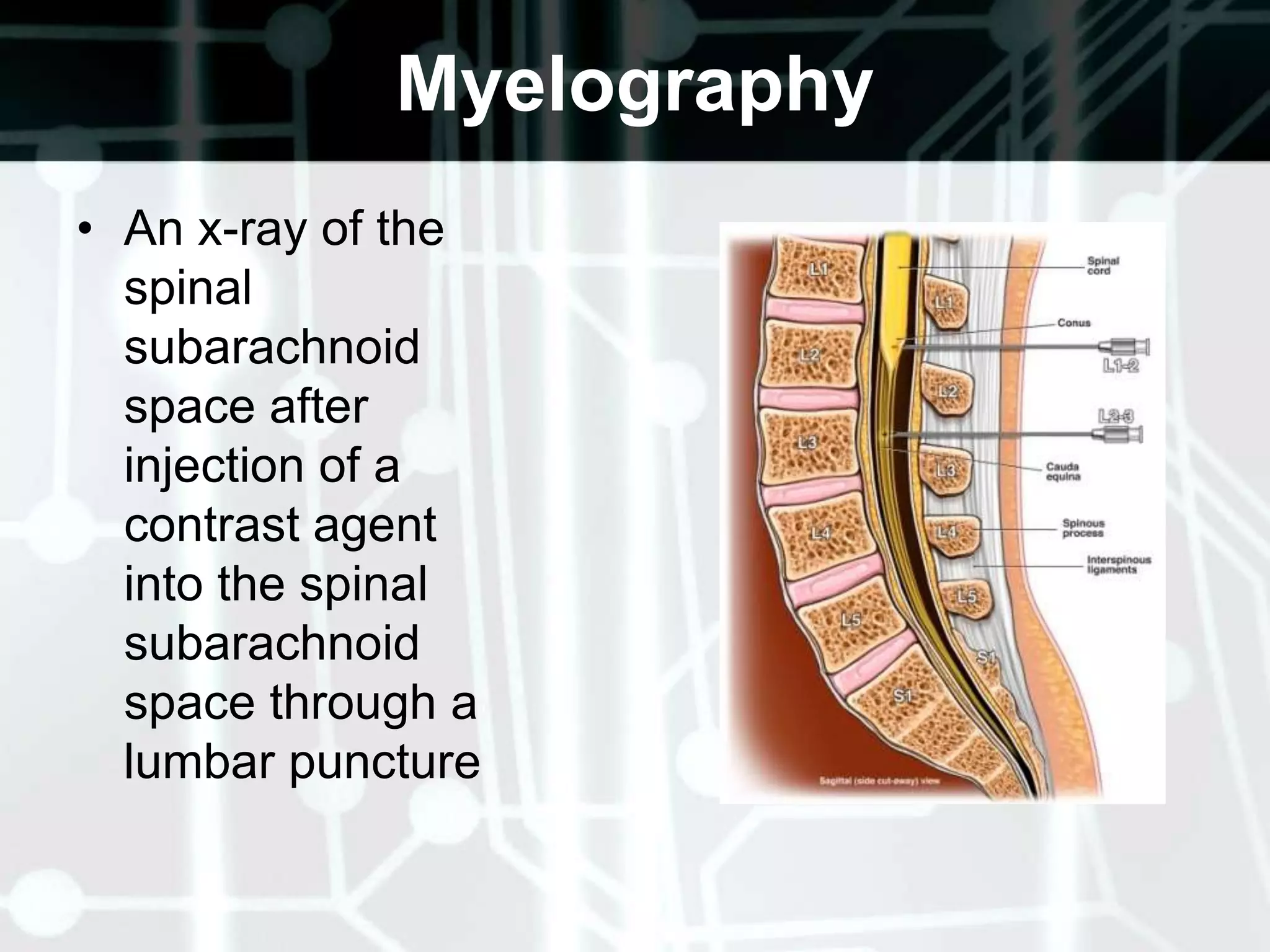
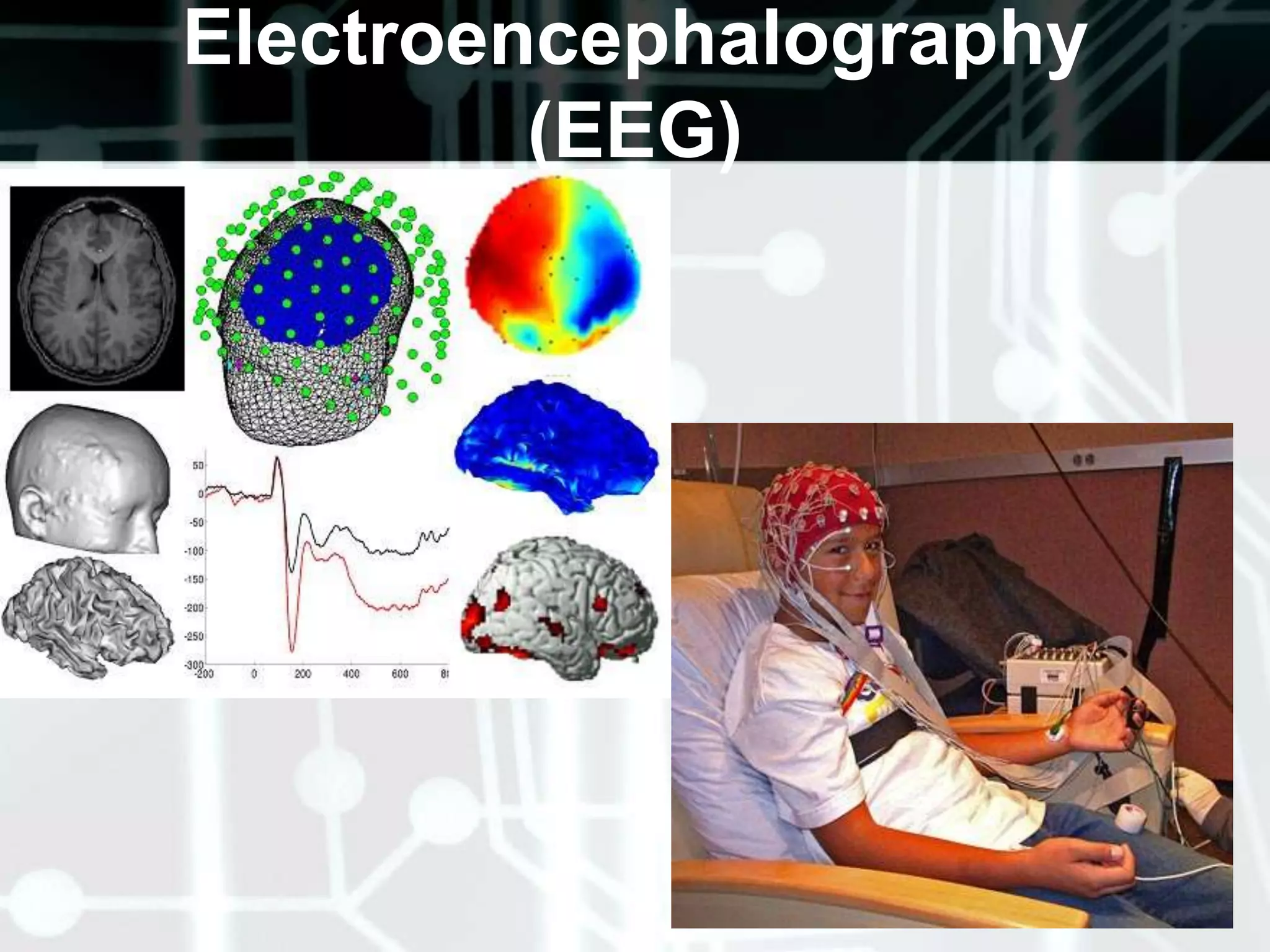
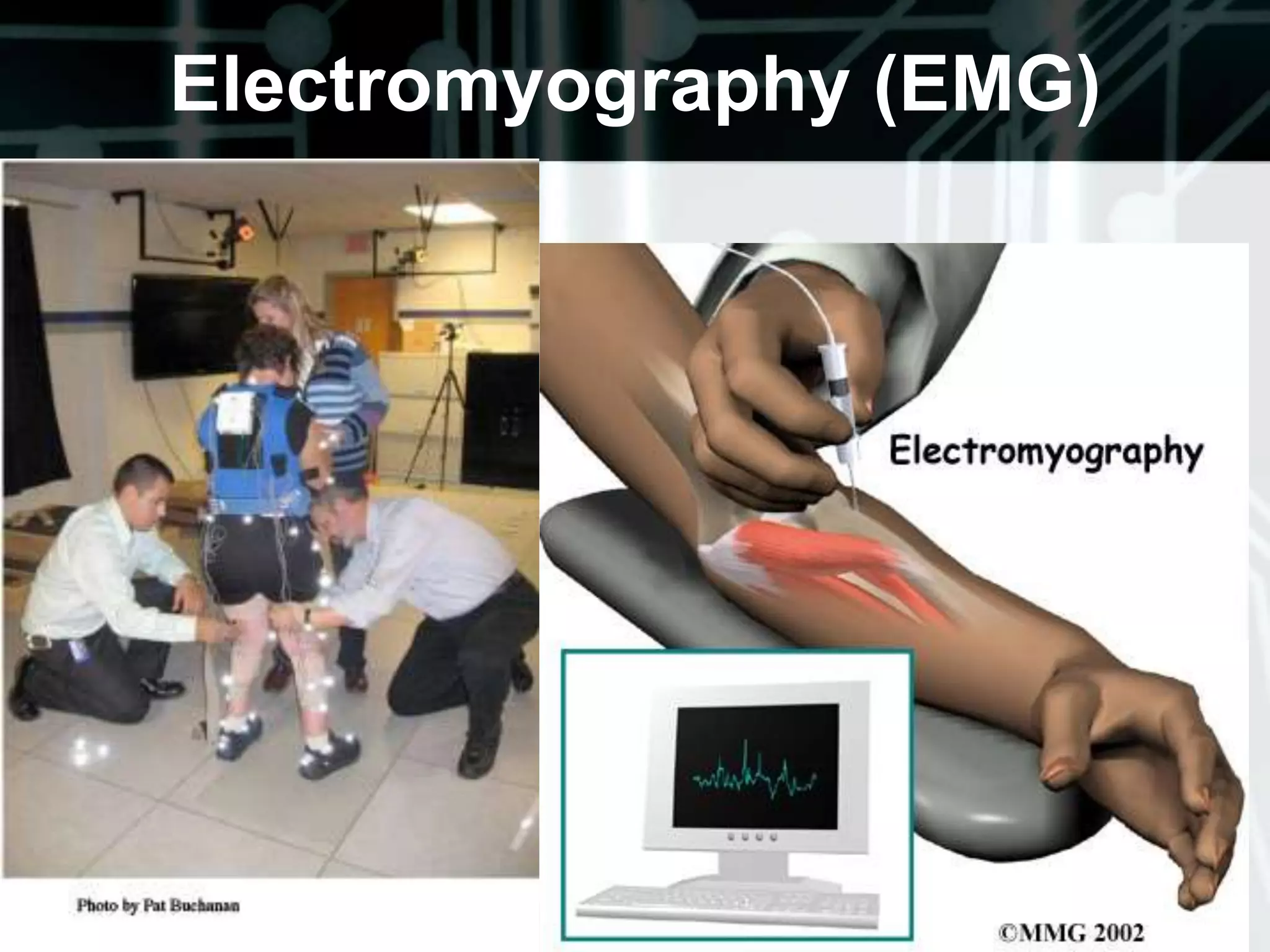
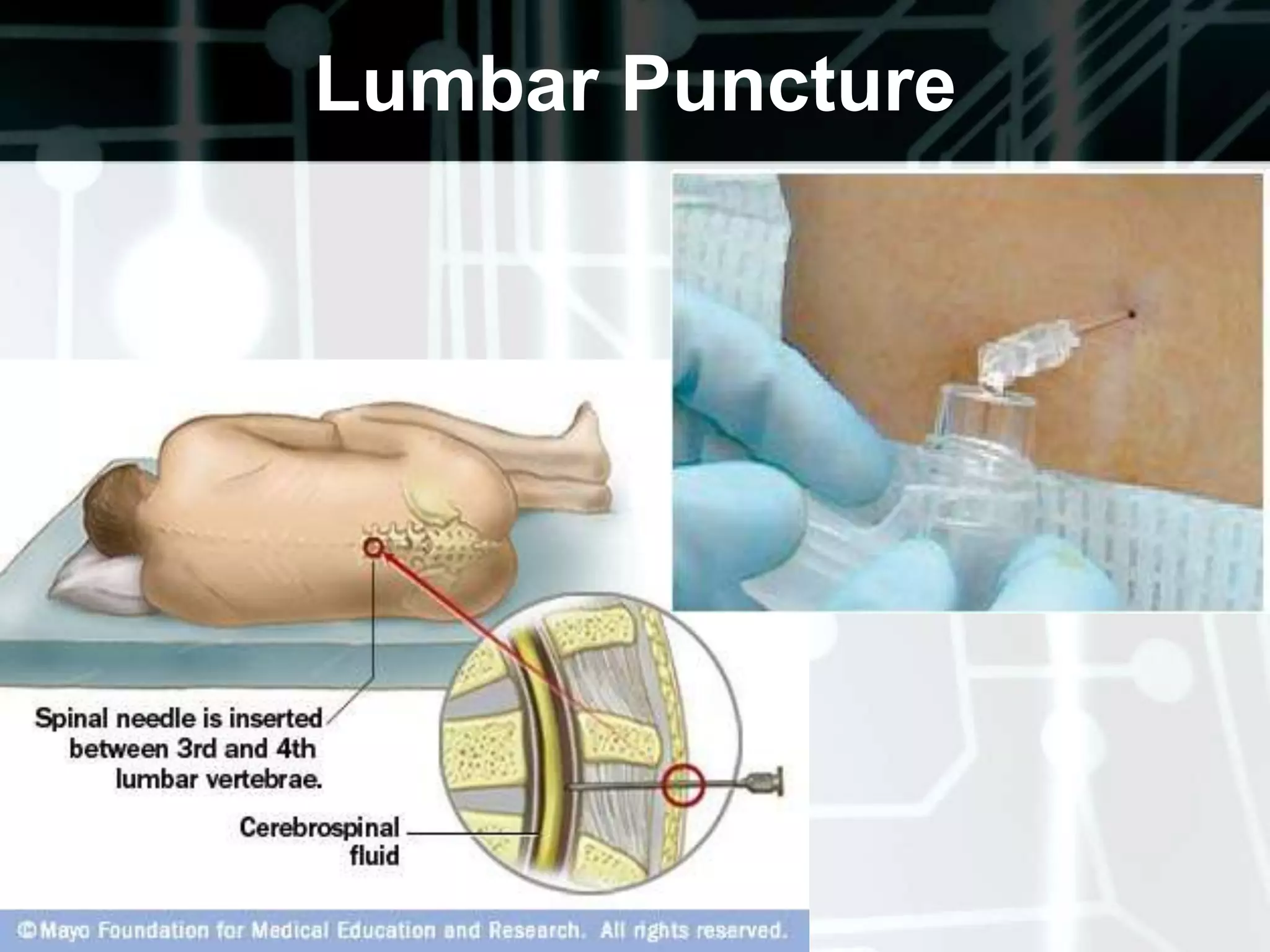
The document provides an overview of performing a neurological examination, which includes obtaining a thorough health history, conducting a physical exam assessing five components (cerebral function, cranial nerves, motor system, sensory system, and reflexes), and ordering diagnostic tests. The physical exam progresses from higher levels of cortical function to lower levels and tests things like mental status, cranial nerves, muscle strength, coordination, balance, reflexes, and sensory function. Common diagnostic tests mentioned are CT, MRI, EEG, EMG, lumbar puncture, and CSF analysis.