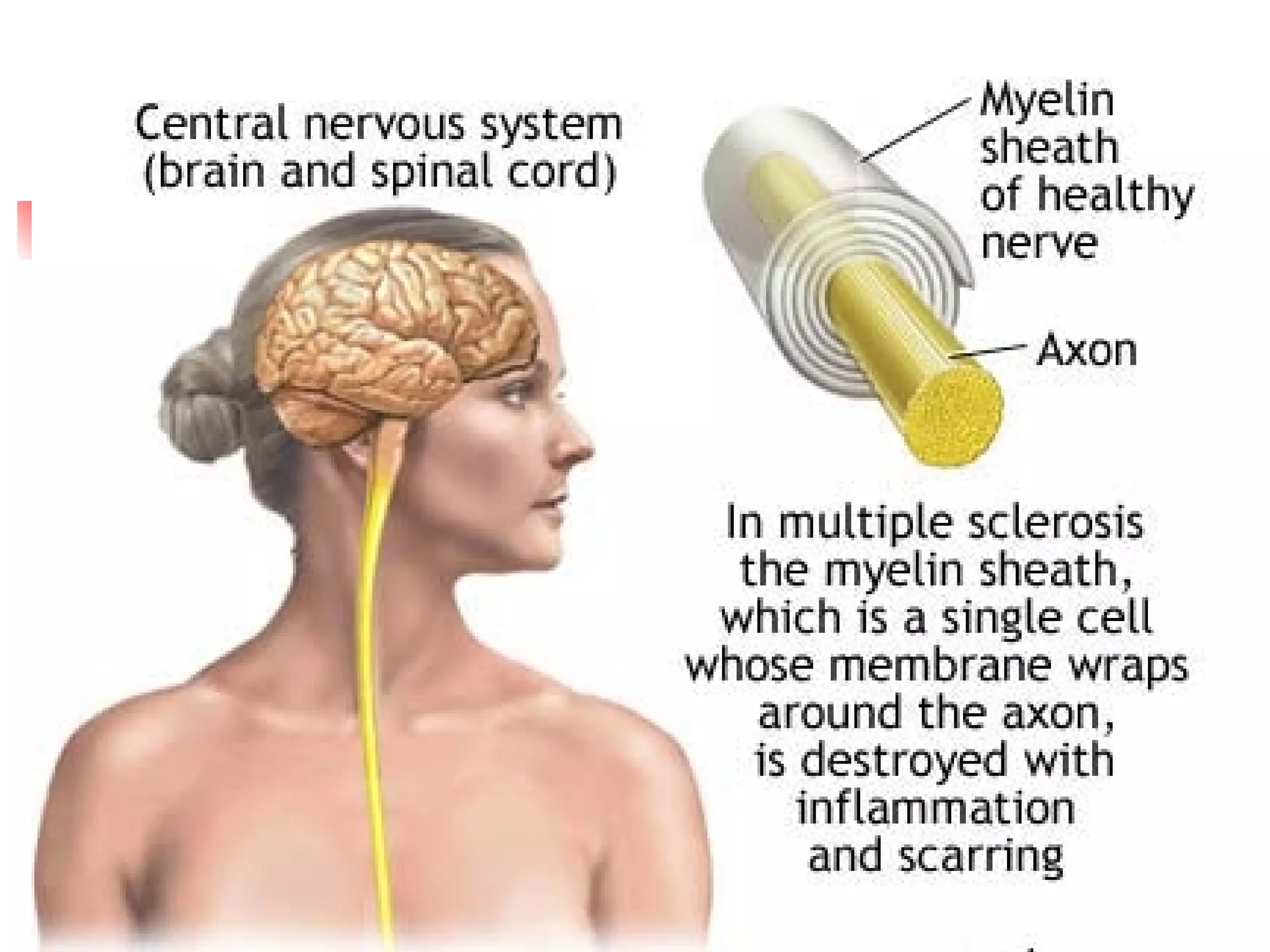
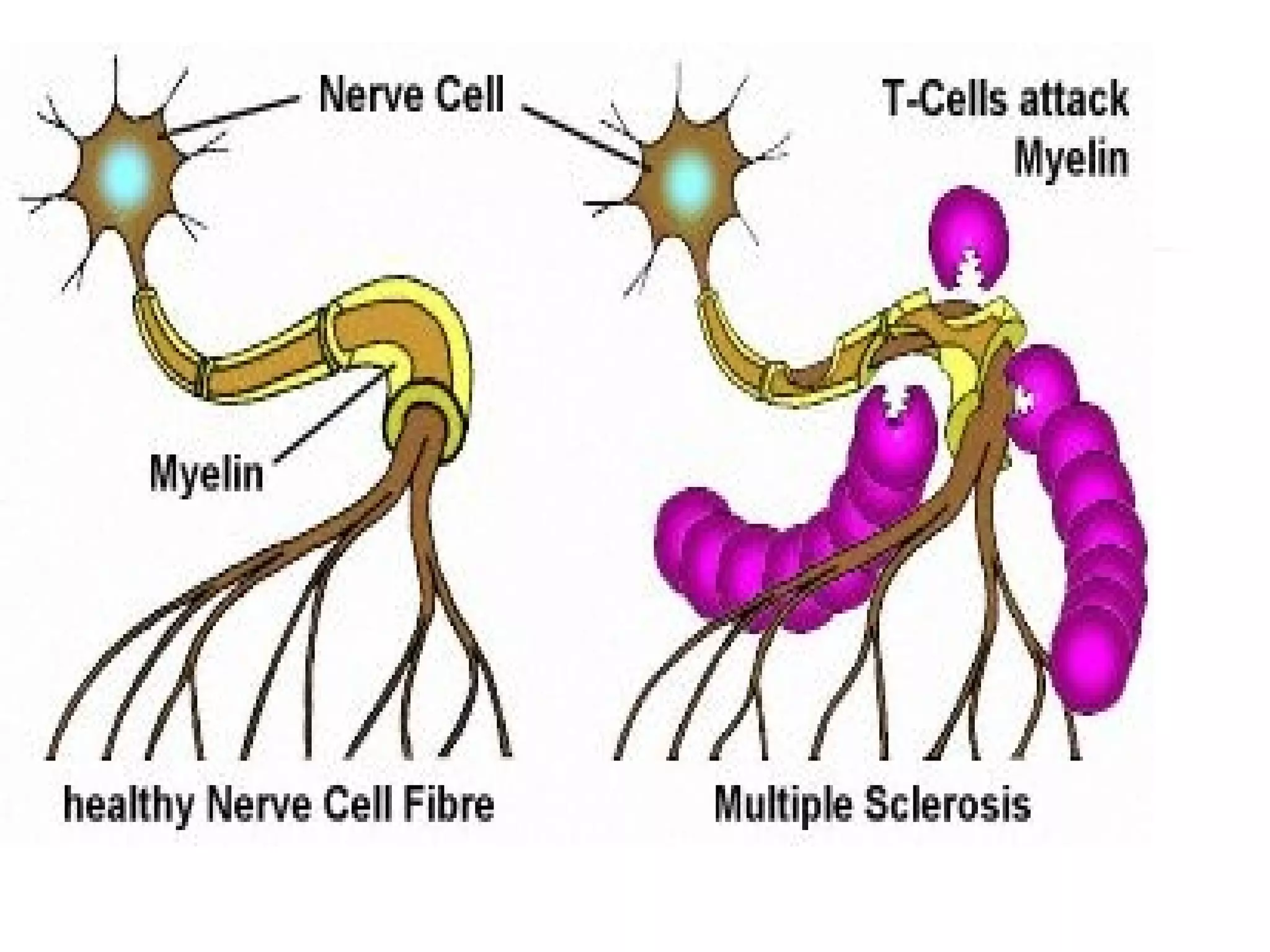
Multiple sclerosis is an autoimmune disease that destroys the myelin sheath protecting nerve fibers in the central nervous system. It causes symptoms like visual problems, motor dysfunction, fatigue, and mood changes. Diagnosis involves MRI and lumbar puncture. Nursing care focuses on promoting mobility, preventing injuries, managing symptoms, and strengthening coping.
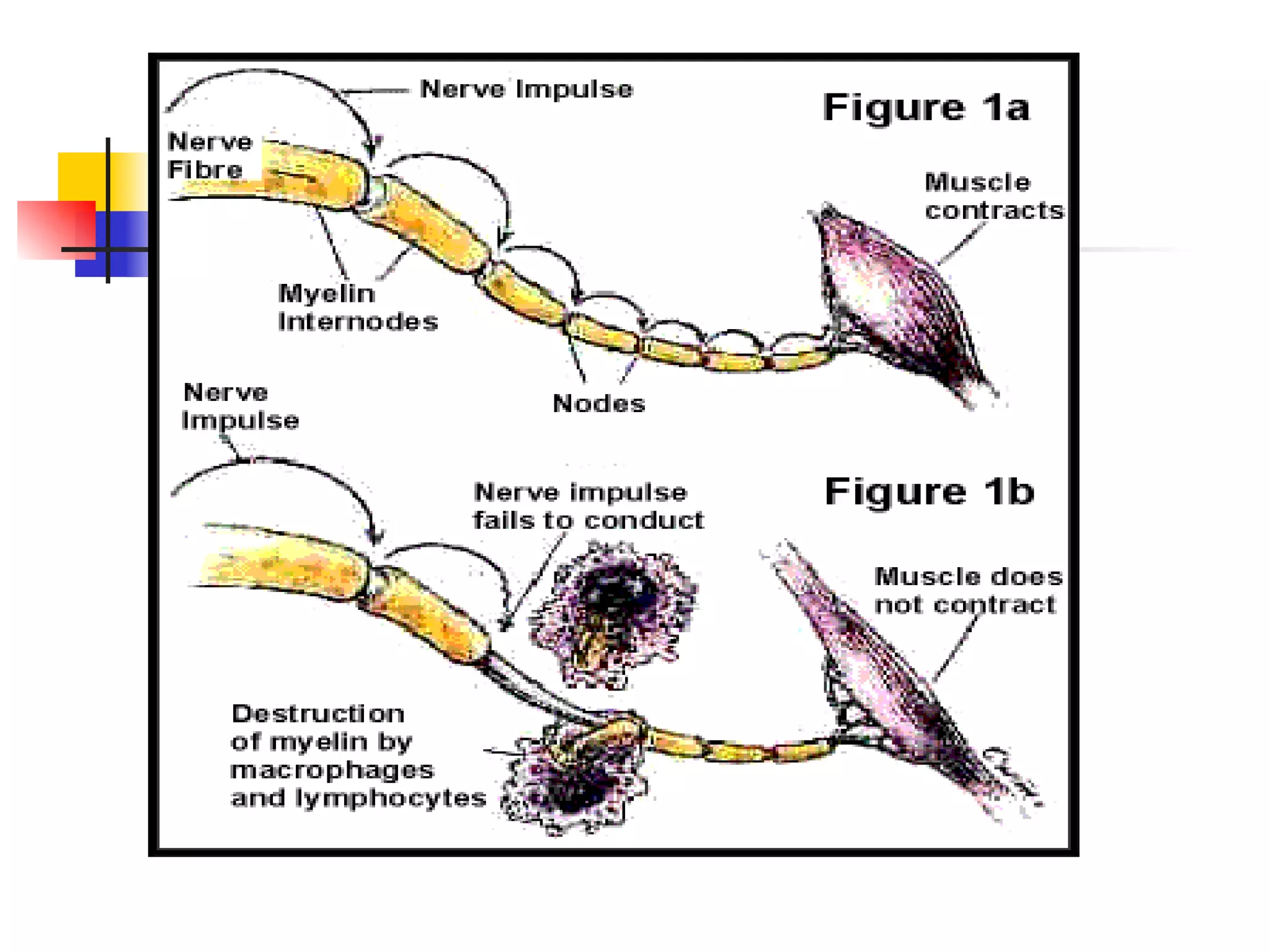
Guillain-Barré syndrome is an autoimmune disorder where the body's immune system attacks the peripheral nervous system, causing muscle weakness and sometimes paralysis. It is usually triggered by a viral or bacterial infection. Nursing care includes maintaining respiratory function, enhancing physical mobility, providing adequate nutrition, and managing complications.
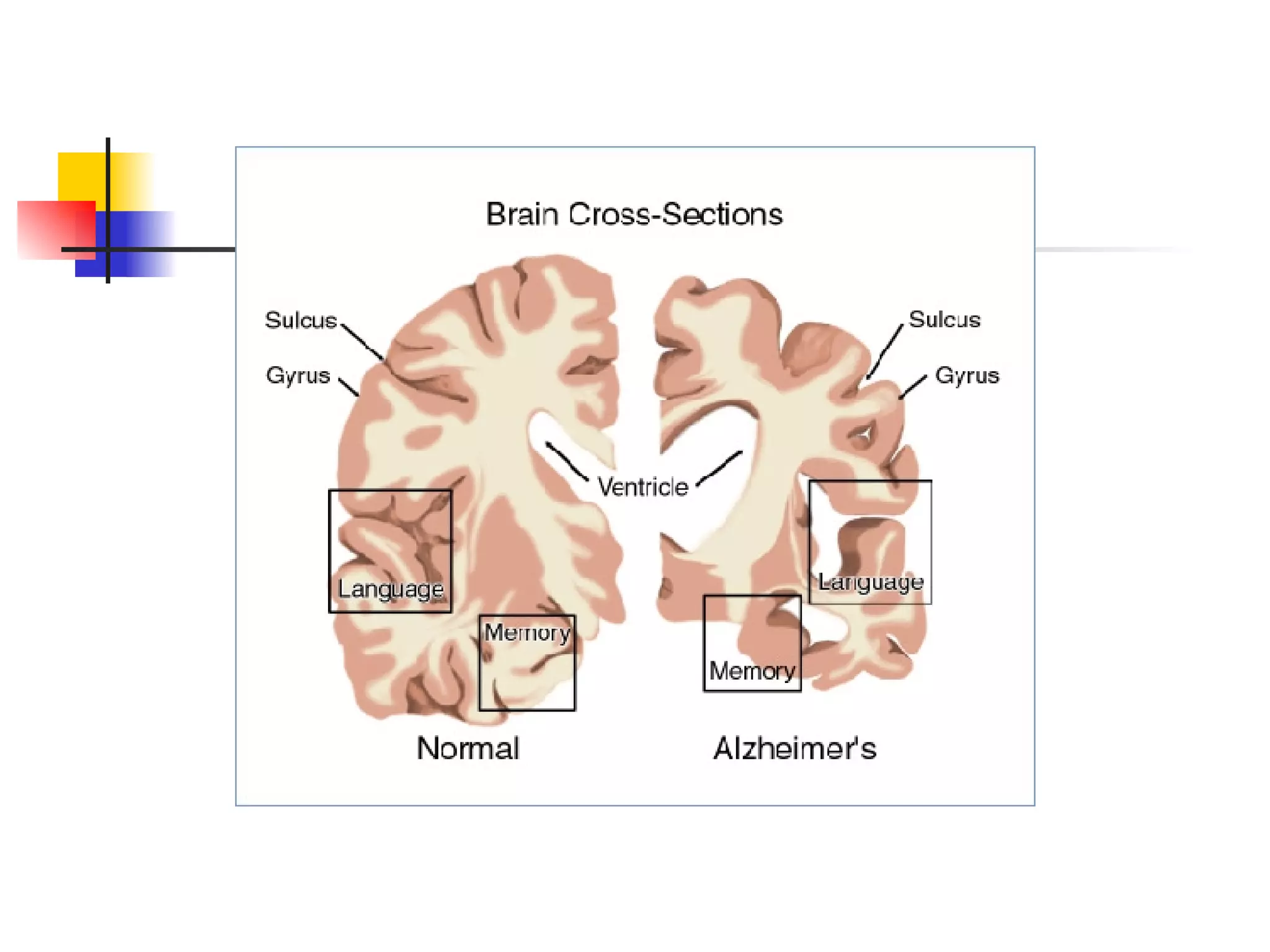
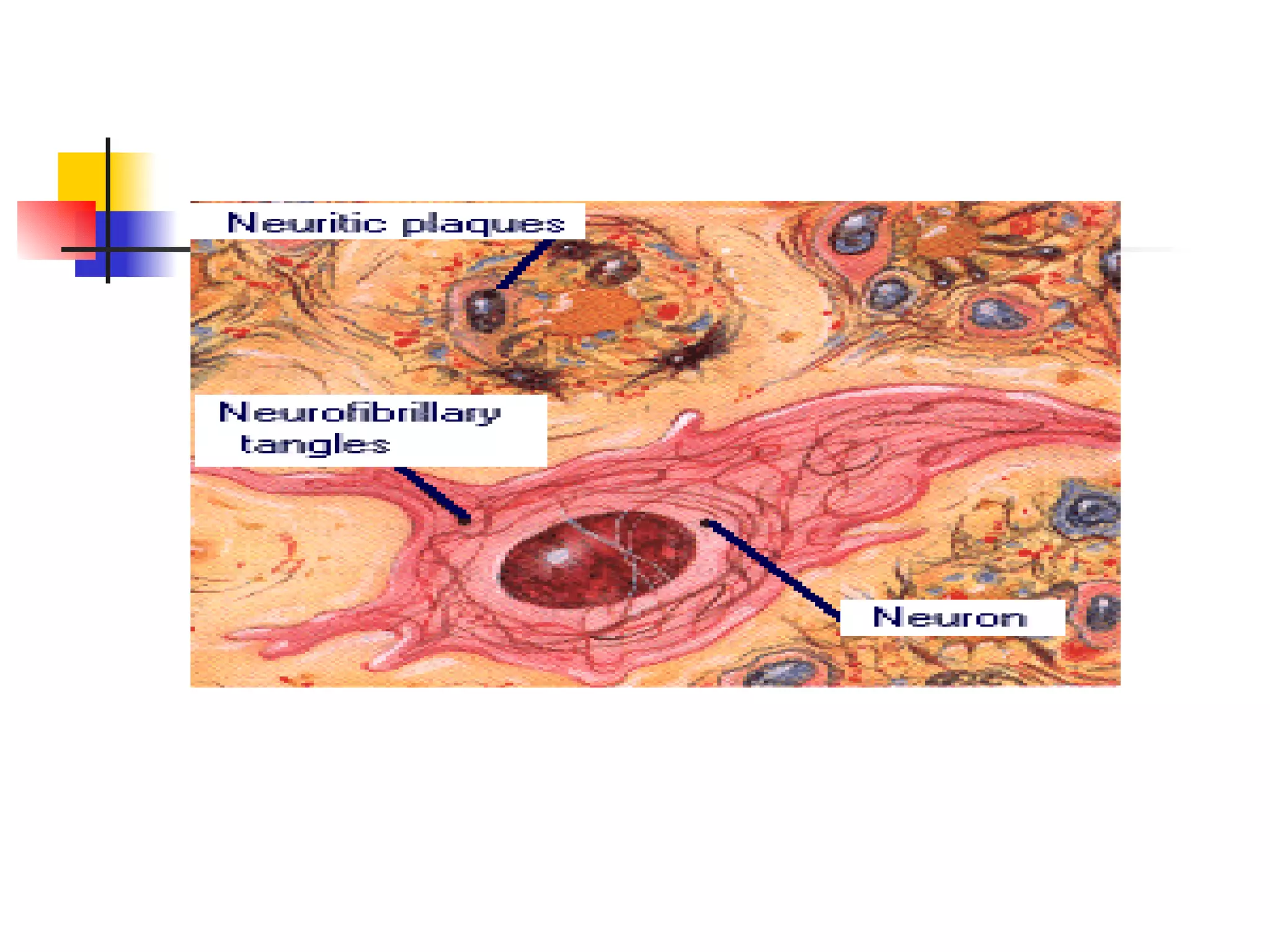
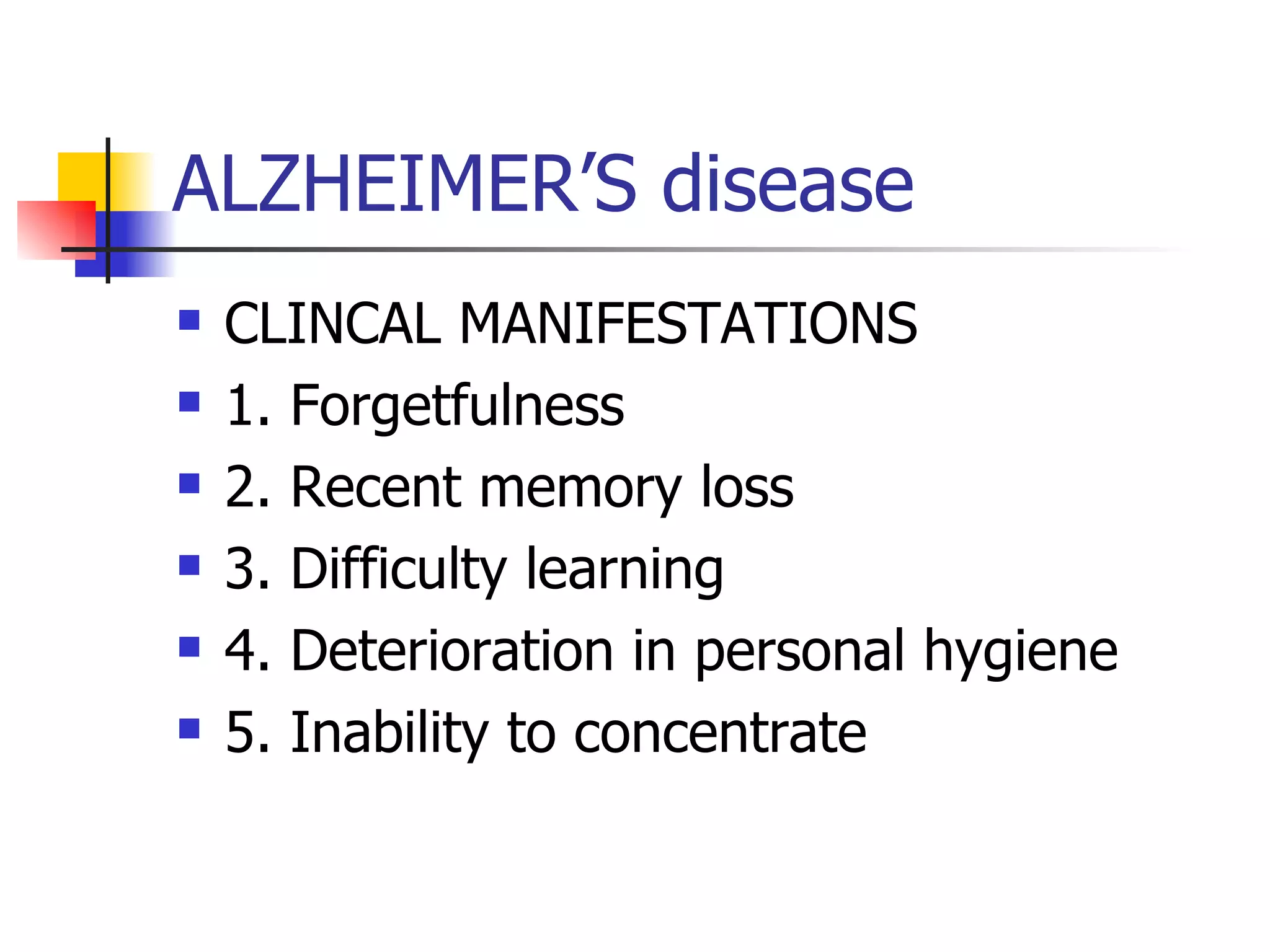
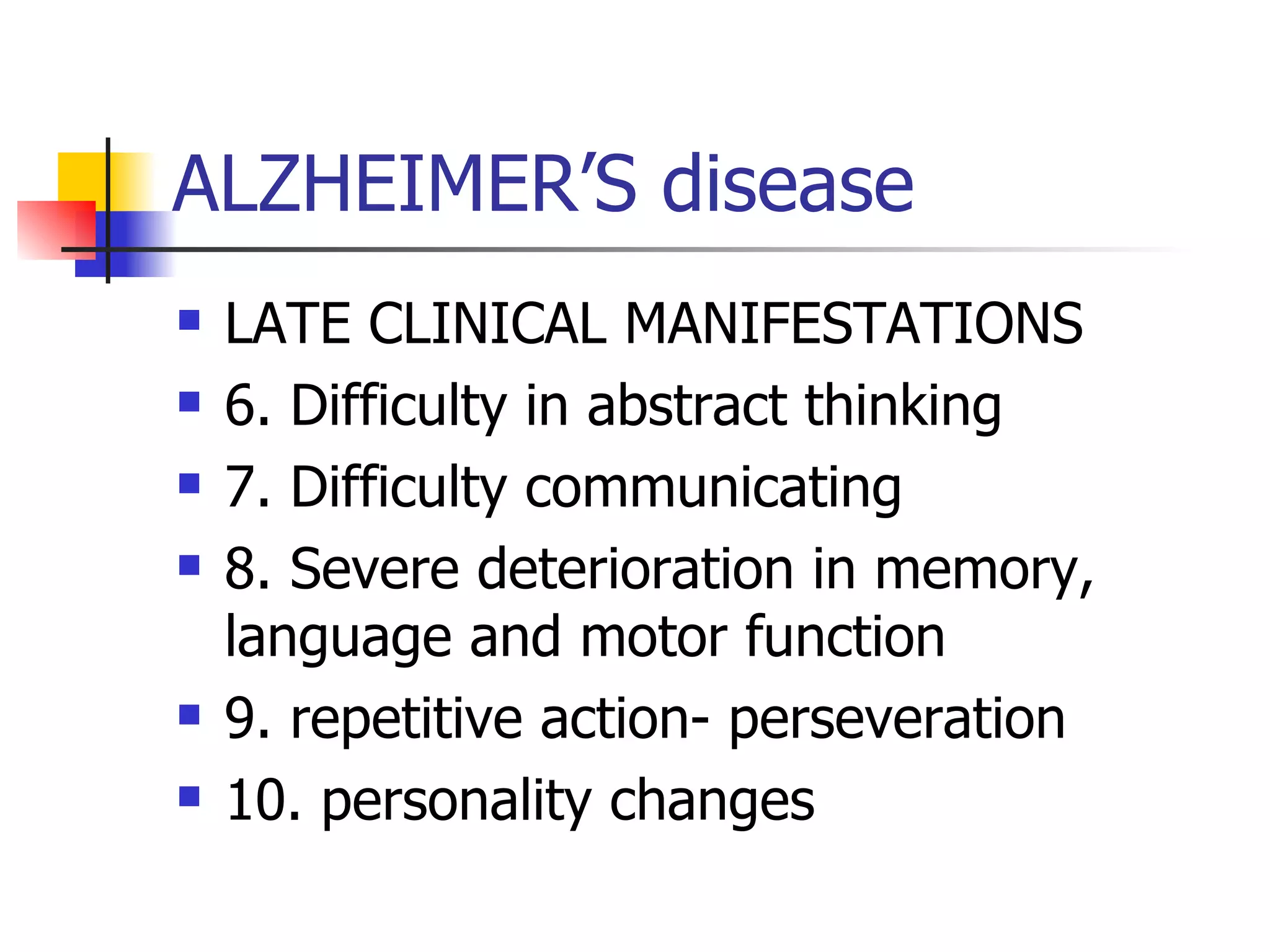
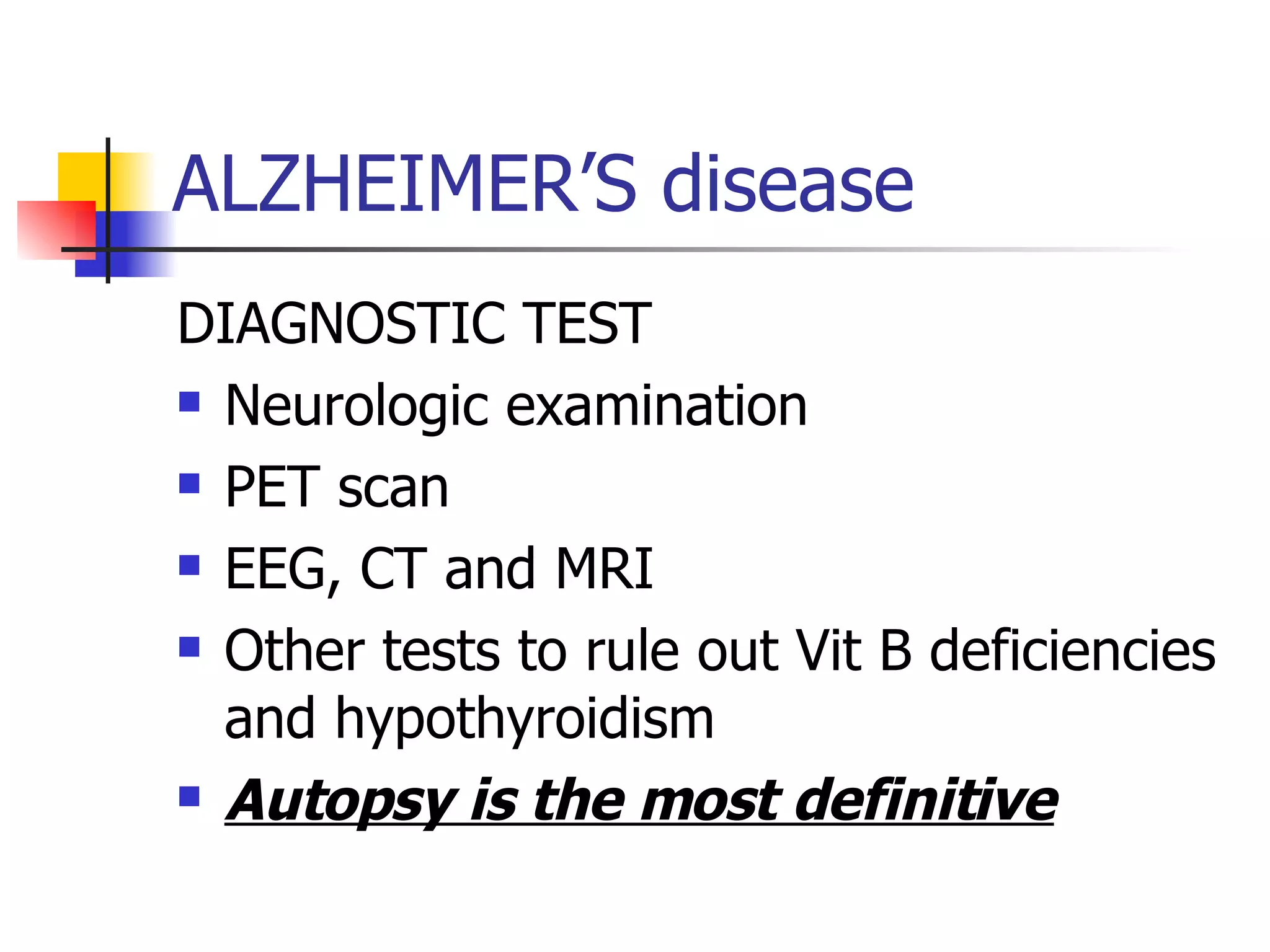
Alzheimer's disease is a progressive brain disorder causing cognitive decline. Sympt