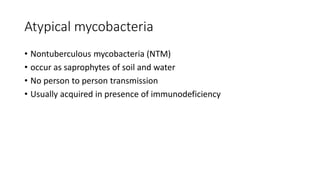
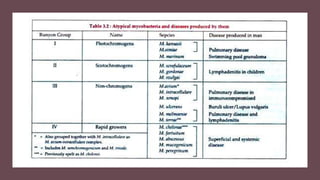
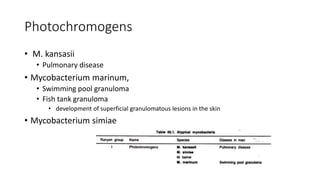
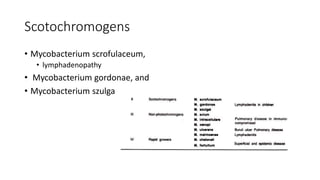
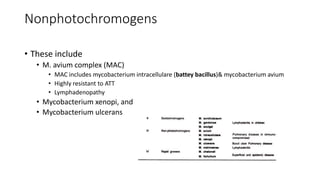
- Atypical mycobacteria include nontuberculous mycobacteria found in the environment that can cause disease in humans under certain conditions.
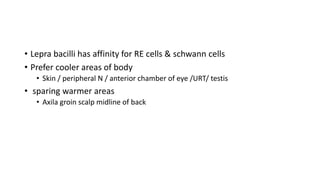
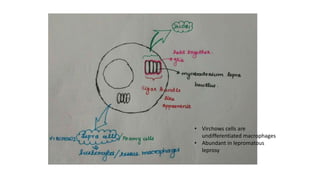
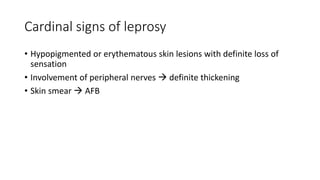
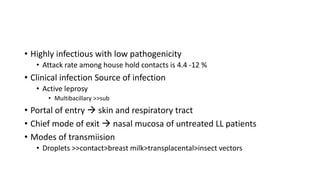
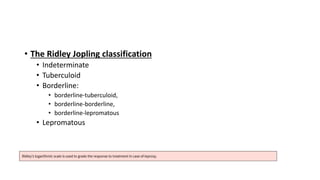
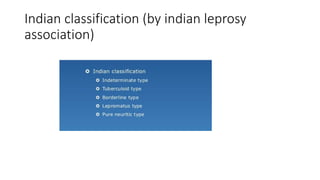
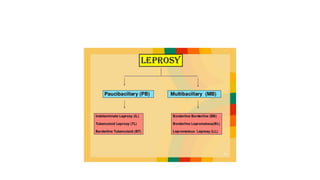
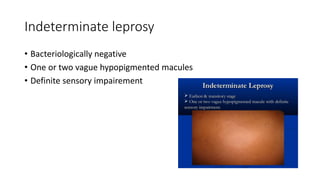
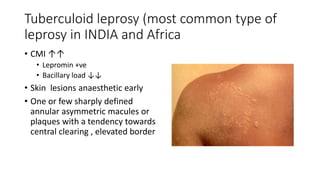
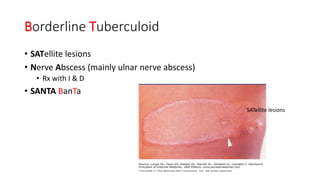
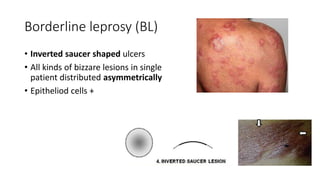
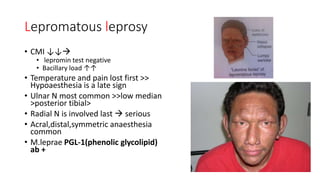
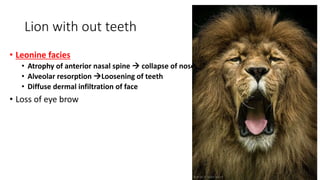
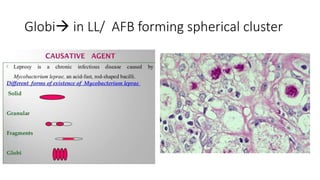
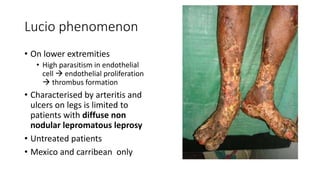
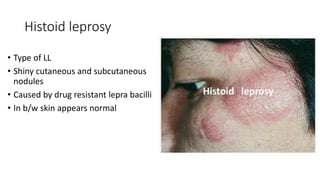
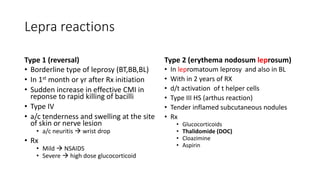
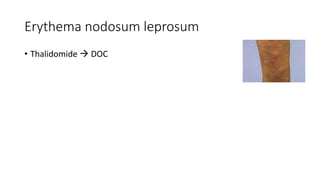
- Mycobacterium leprae causes leprosy (Hansen's disease), with a spectrum of clinical manifestations depending on immune response from tuberculoid to lepromatous leprosy.
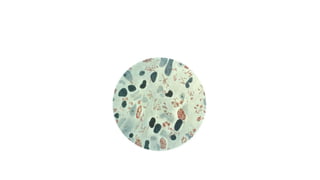
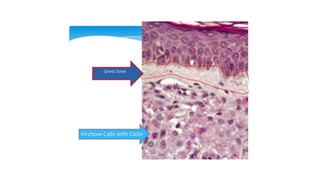
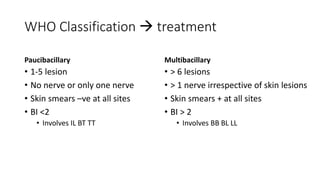
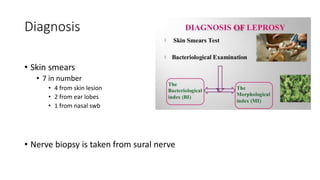
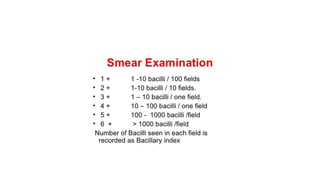
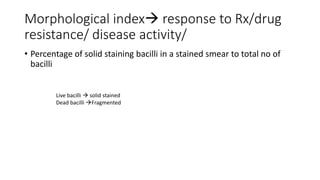
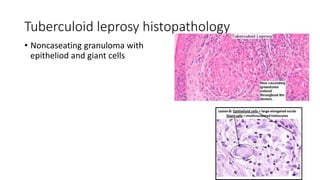
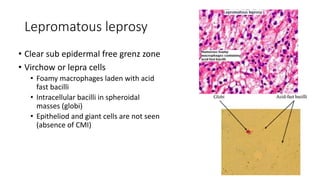
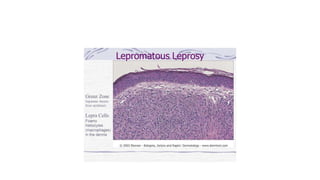
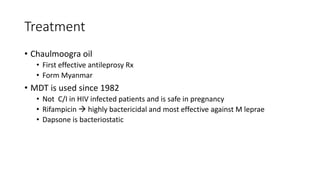
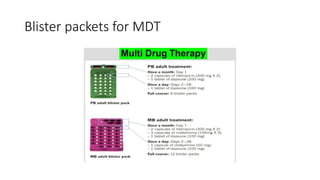
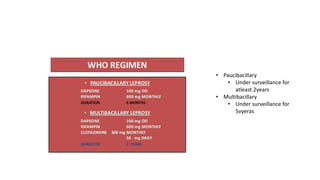
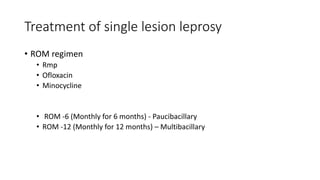
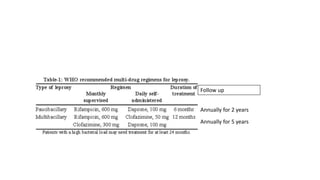
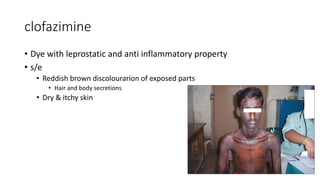
- Diagnosis involves skin smears and biopsy showing acid-fast bacilli. Treatment is multidrug therapy including dapsone, rifampin, and clofazimine.