This document provides information about Mycobacteria, including:
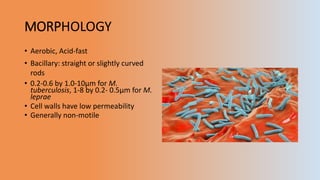
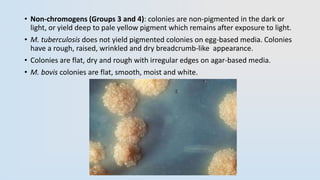
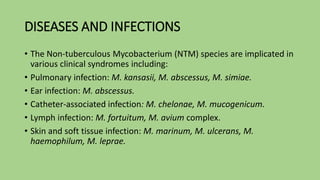
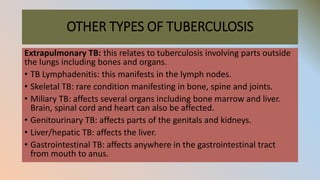
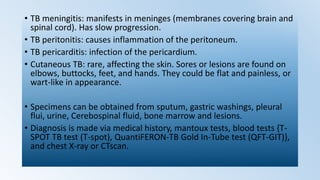
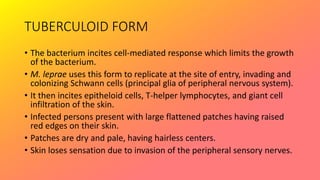
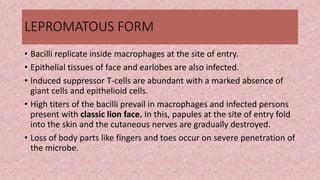
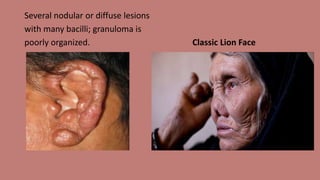
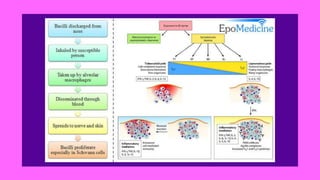
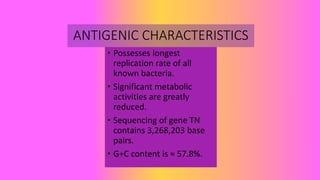
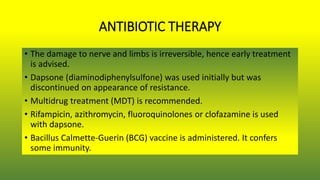
- They are acid-fast bacteria that cause diseases like tuberculosis and leprosy.
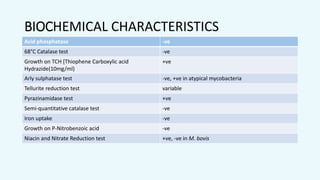
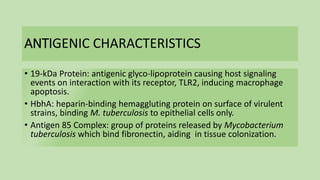
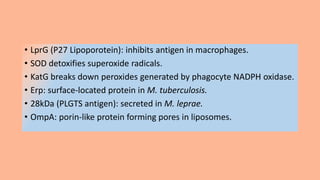
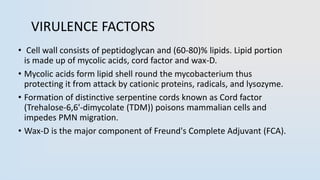
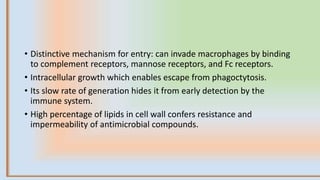
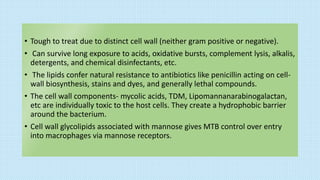
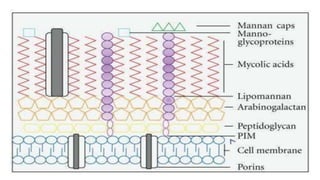
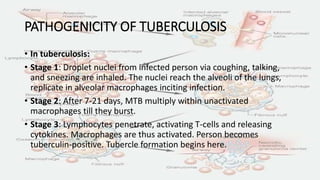
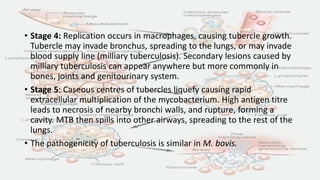
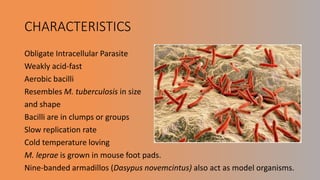
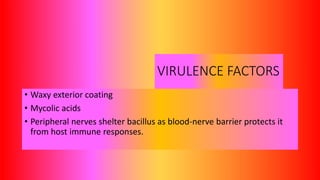
- Mycobacteria have a thick, waxy cell wall that makes them resistant to antibiotics and able to survive inside host cells.
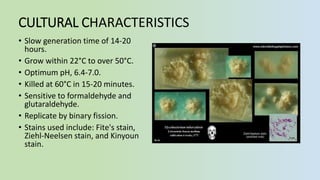
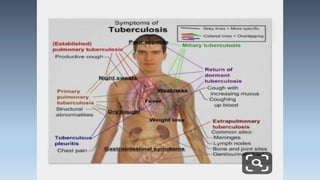
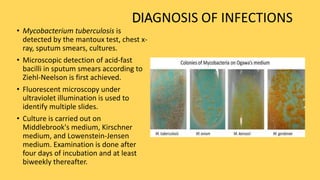
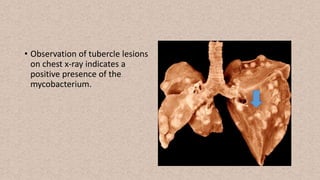
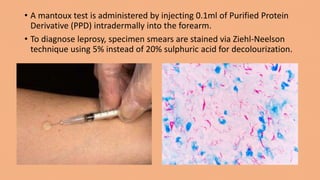
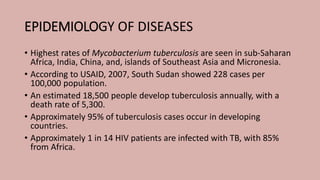
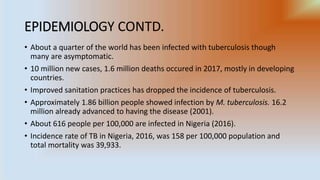
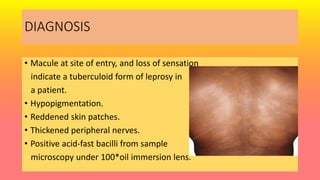
- Diseases are diagnosed through microscopy, culture, mantoux tests, and chest x-rays. High rates of tuberculosis infection occur in developing regions of Africa, Asia, and the Pacific.