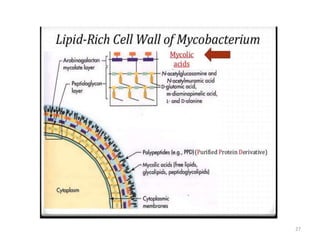
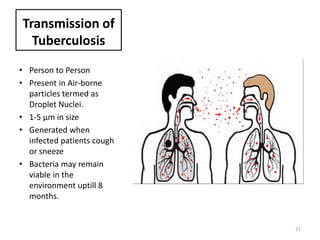
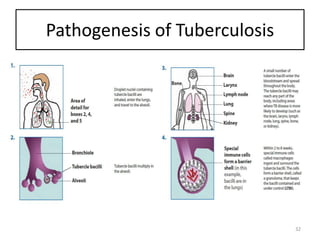
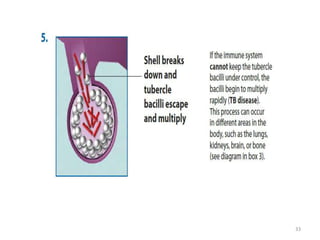
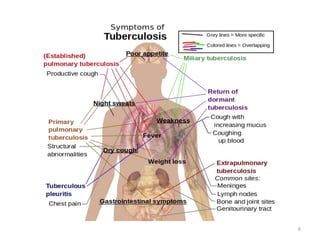
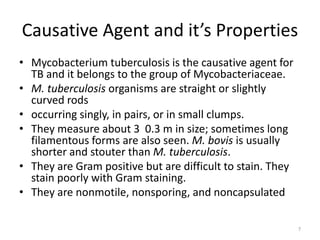
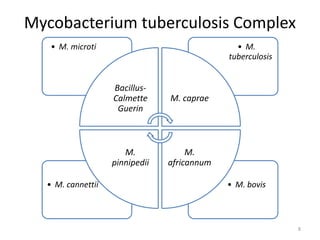
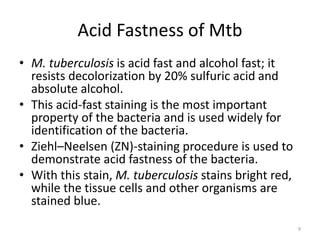
This document covers tuberculosis (TB), focusing on its causative agent, Mycobacterium tuberculosis, its types, symptoms, and pathogenesis. It explores the biology and cultural requirements of the bacteria, including its growth characteristics and biochemical properties, as well as host immunity and transmission methods. Additionally, it discusses the significance of tuberculin testing and the role of human hosts in the infection's spread.
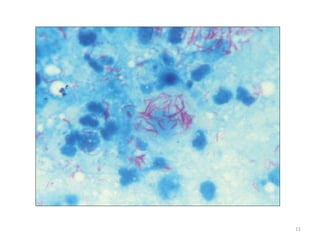
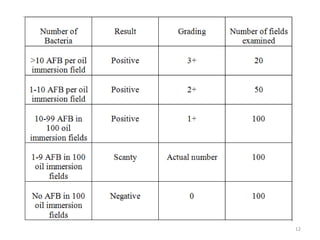
![C] Ziehl- Neelsen Staining and Grading
10](https://image.slidesharecdn.com/tuberculosis-151002080343-lva1-app6891/85/Tuberculosis-Diagnosis-and-Treatment-10-320.jpg)
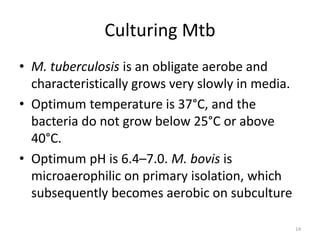
![Culture on solid media
• The examples of solid media are
(i) egg-containing media (Lowenstein–Jensen [LJ]
medium,Petragnani and Dorset egg medium)
(ii) blood-containing media (Tarshis medium),
serum-combining media (Loeffler’s serum slope),
(iii) potato-based media (Pawlowsky medium).
• On these media, M. tuberculosis produces dry,
rough, raised, and irregular colonies with a
wrinkled surface.
16](https://image.slidesharecdn.com/tuberculosis-151002080343-lva1-app6891/85/Tuberculosis-Diagnosis-and-Treatment-16-320.jpg)