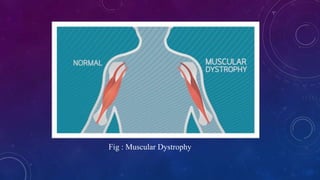
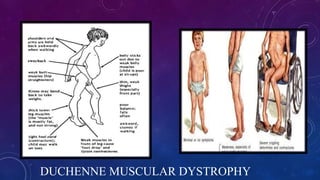
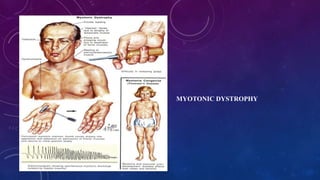
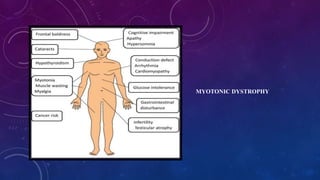
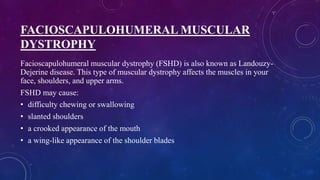
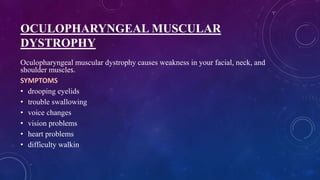
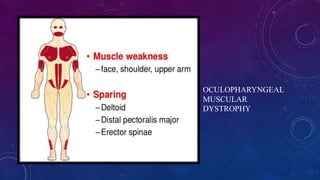
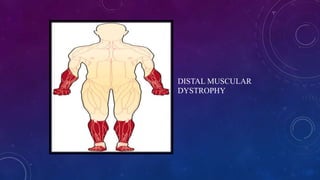
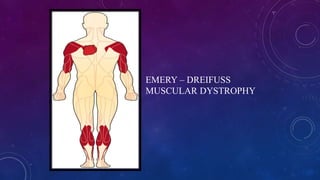
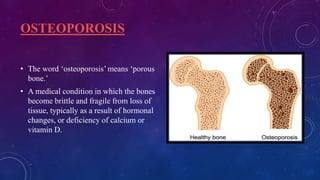
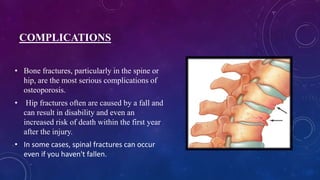
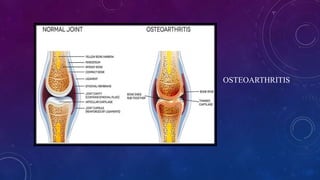
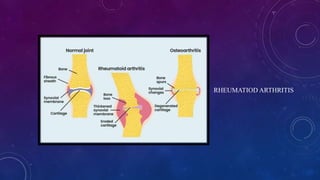
This document provides information about musculoskeletal system disorders (MSDs). It discusses that MSDs affect muscles, bones, and joints, causing symptoms like pain, stiffness, and swelling. Common MSDs include muscular dystrophy, osteoporosis, and arthritis. The document then goes on to describe different types of muscular dystrophies in more detail, including their symptoms, causes, diagnosis, and treatment. It also discusses osteoporosis and its risk factors. In summary, the document outlines what MSDs are, common types like muscular dystrophies and osteoporosis, and their symptoms and treatment options.