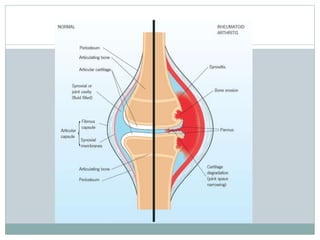
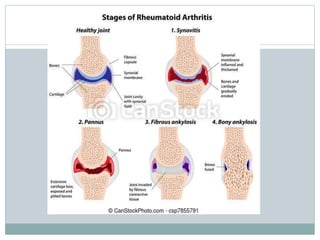
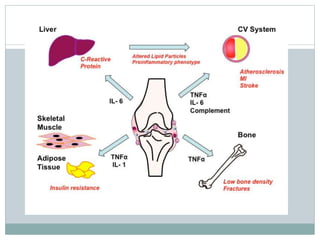
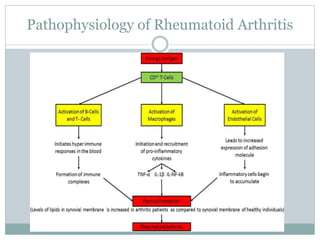
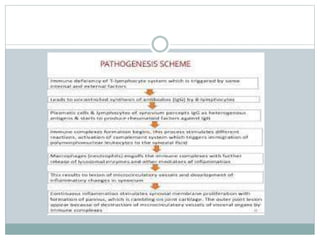
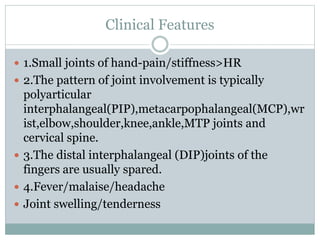
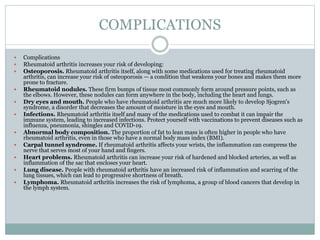
Rheumatoid arthritis is a chronic inflammatory disease that primarily affects the joints, especially small joints in the hands and feet. It is more common in women and is caused by genetic and autoimmune factors. Symptoms include pain, stiffness, swelling in small and large joints. Over time, joint deformities can develop if not treated. Diagnostic tests include blood tests, x-rays, MRI and synovial fluid analysis. Treatment involves medications like NSAIDs, DMARDs, steroids and biologics to reduce inflammation and prevent joint damage. Lifestyle changes and physical therapy can also help manage symptoms. Complications may include osteoporosis, lung and heart disease if not properly treated.