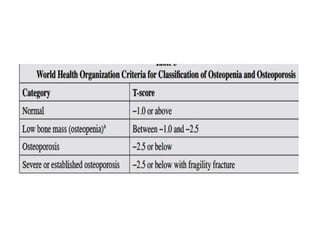
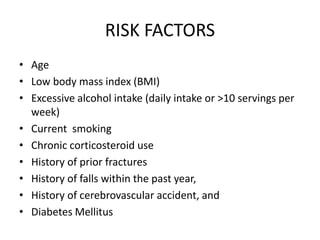
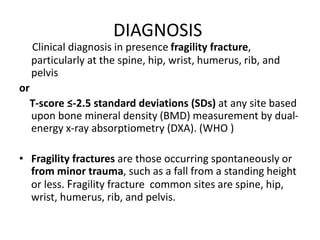
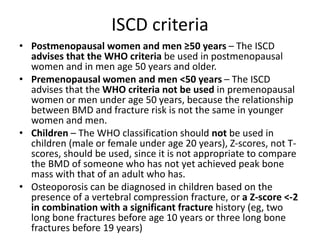
This document provides an overview of osteoporosis. It defines osteoporosis as a skeletal disease characterized by low bone mass and deterioration of bone tissue, leading to increased bone fragility and risk of fracture. Key risk factors include age, low body weight, smoking, excess alcohol, corticosteroid use, and prior fractures. Diagnosis involves assessing bone mineral density via dual-energy x-ray absorptiometry (DXA) scanning or estimating fracture risk using FRAX. Treatment focuses on lifestyle modifications like exercise, calcium and vitamin D supplementation, as well as pharmacological therapies like bisphosphonates.



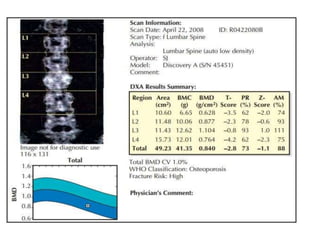

![LABORATORY EVALUATION
• Biochemistry profile (especially calcium, phosphorous,
albumin, total protein, creatinine, liver enzymes including
alkaline phosphatase, electrolytes)
• 25-hydroxyvitamin D (25[OH]D)
• Complete blood count (CBC)
• If the diagnosis of osteoporosis is based upon the
presence of a fragility fracture, obtain a BMD
measurement (dual-energy x-ray absorptiometry
[DXA]), performed on a nonurgent basis, for
quantitative assessment of bone density and to monitor
response to therapy.](https://image.slidesharecdn.com/osteoporosis-220604142727-2385f9a5/85/Osteoporosis-25-320.jpg)
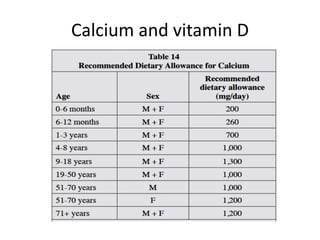
![• Dietary calcium may be preferred over supplemental
calcium and that total calcium intake should not exceed
1,500 mg/day .Increasing calcium intake beyond the
recommended levels has lead to increased risk of
cardiovascular disease, stroke and nephrolithiasis .
• Recommended intake of vitamin D is at least
1,000 IU of per day for adults aged 50 years and
older.
• Adults who are vitamin D insufficient or deficient
(serum 25[OH]D 20 to 29 or <20 ng/mL, respectively)
maybe treated with 5,000 IU vitamin D3 daily for 8 to 12
weeks to achieve a 25(OH)D blood level >30 ng/mL.](https://image.slidesharecdn.com/osteoporosis-220604142727-2385f9a5/85/Osteoporosis-30-320.jpg)
![Assessment before starting bisphosphonates
1. Biochemical
• Calcium
• 25-hydroxyvitamin D (25[OH]D)
• Creatinine
• For both oral and intravenous (IV)
bisphosphonates, correction of hypocalcemia
and/or vitamin D deficiency (to at least 20 ng/mL
[50 nmol/L]) is necessary prior to administration
2. Assess comorbidities history to detect any abnormalities
of the esophagus (stricture, achalasia) and an inability to
remain upright for at least 30 to 60 minutes.
3. Plans for invasive dental procedures developing
osteonecrosis of the jaw.](https://image.slidesharecdn.com/osteoporosis-220604142727-2385f9a5/85/Osteoporosis-34-320.jpg)
![DURATION OF THERAPY
• Low risk for fracture – For patients at low risk for fracture in
the near future (eg, stable bone mineral density [BMD], no
previous vertebral or hip fractures), discontinuing the drug
(after three years for zoledronic acid, five years for
alendronate or risedronate)
• High risk for fracture – For patients at highest risk for fracture
(history of osteoporotic fracture before or during therapy, T-
score below -3.0 in the absence of fractures) who are taking
alendronate or risedronate, continuing therapy for up to 10
years
• Drug holiday because bisphosphonates accumulate and may
have a prolonged residence time in bone (and residual
therapeutic effect after stopping), “bisphosphonate holidays”
may be considered. Drug holiday can be considered after 5
years of stability on oral bisphosphonates or 3 years of IV
zoledronate](https://image.slidesharecdn.com/osteoporosis-220604142727-2385f9a5/85/Osteoporosis-35-320.jpg)