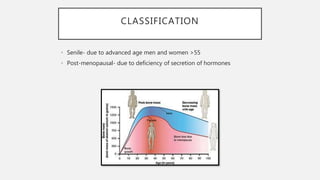
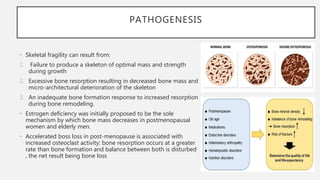
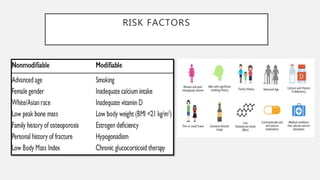
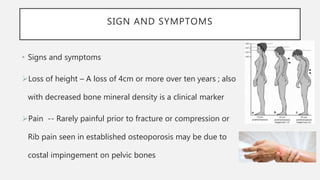
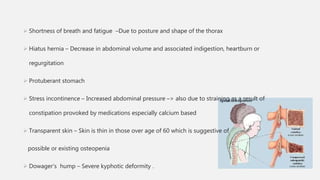
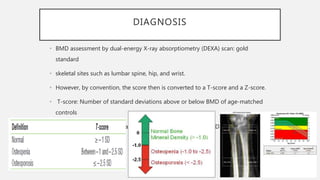
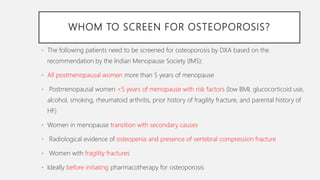
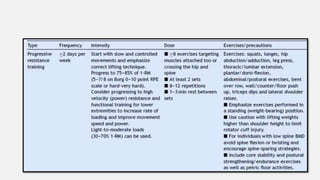
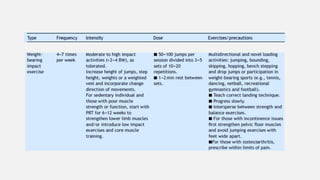
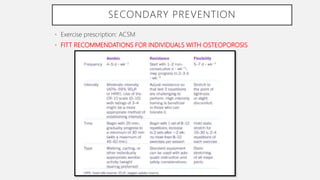
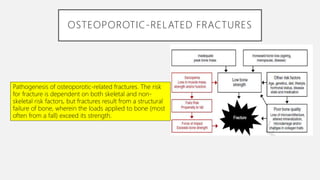
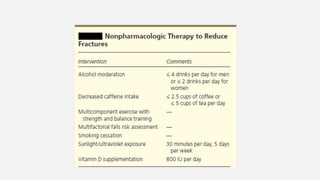
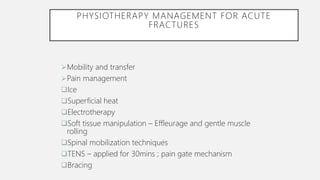
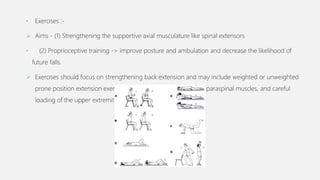
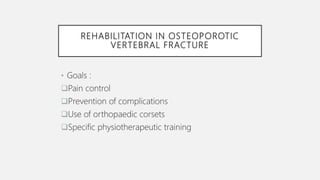
Osteoporosis is a disease characterized by low bone mass and deterioration of bone tissue, leading to increased bone fragility and risk of fractures. It is most common in postmenopausal women and the elderly. Risk factors include advanced age, post-menopause, family history, smoking, excessive alcohol, low body weight and long-term glucocorticoid use. Diagnosis involves assessing bone mineral density through DEXA scan and evaluating fracture risk. Physiotherapy management focuses on exercise to build bone strength, mobility and independence through range of motion, strengthening and balance exercises. Bracing and orthotics are also used following fractures.