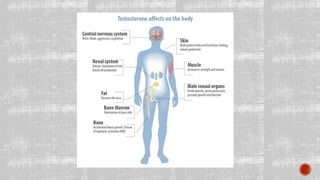
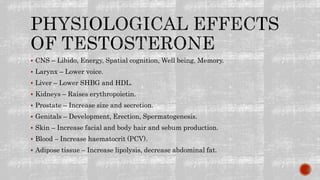
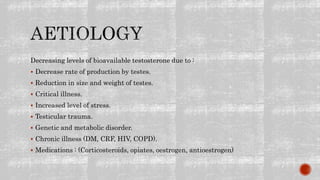
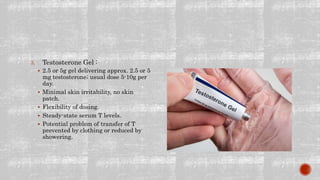
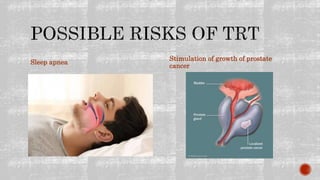
Andropause, also known as male menopause, is the gradual decline in testosterone levels that occurs in men as they age. Unlike female menopause which is sudden, andropause is a slow process resulting in more subtle symptoms. Low testosterone can negatively impact many organ systems and quality of life. Treatment options include lifestyle changes as well as hormone replacement therapy administered through oral, injectable, or transdermal methods. However, testosterone therapy may increase risks for certain health conditions like sleep apnea and prostate issues.