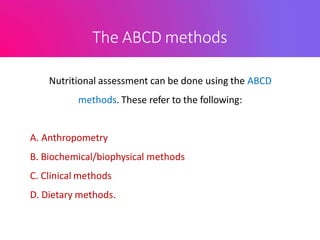
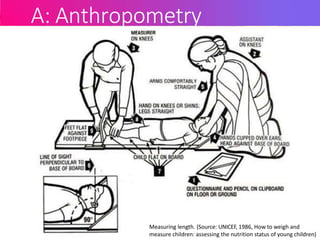
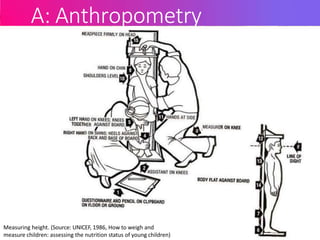
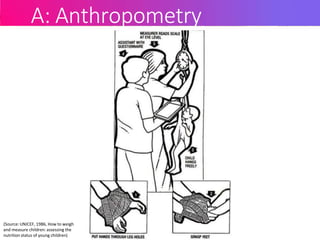
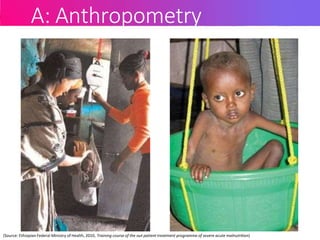
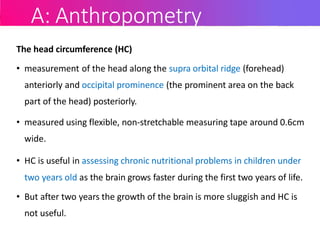
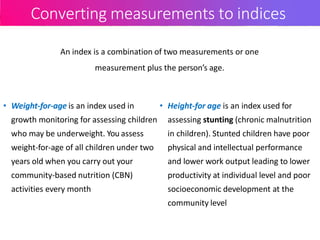
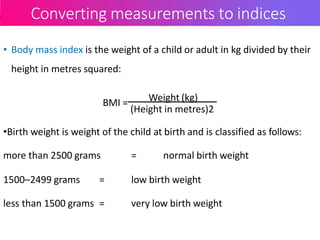
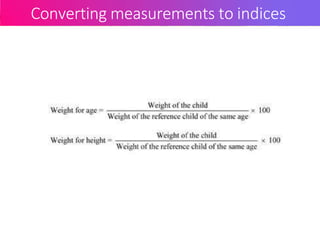
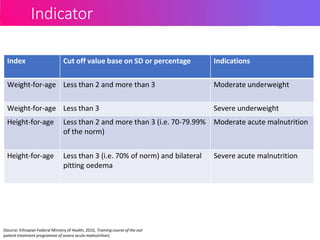
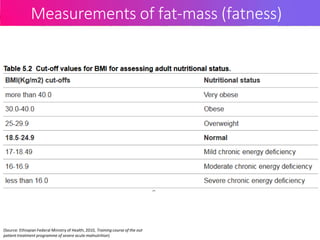
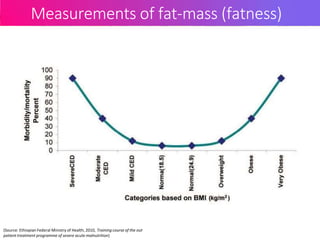
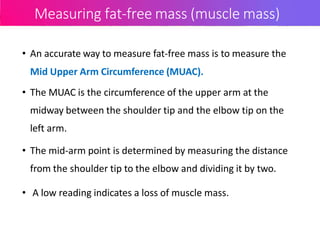
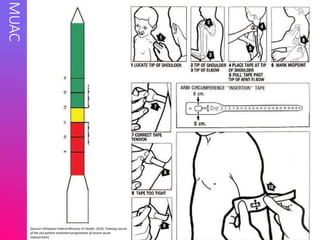
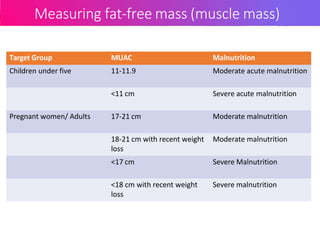
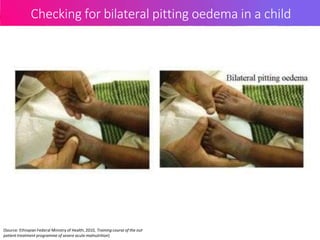
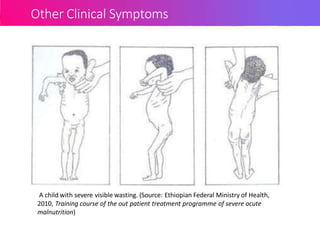
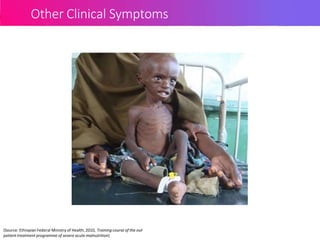
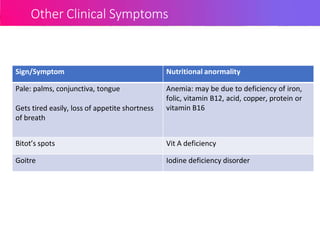
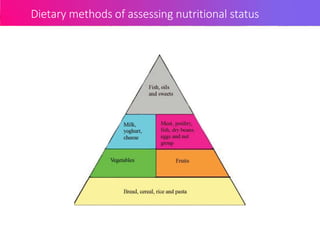
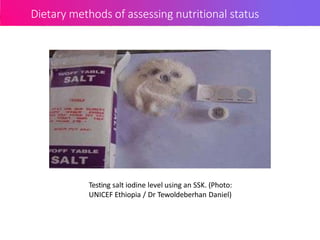
This document discusses methods for assessing nutritional status, including anthropometric, biochemical, clinical, and dietary methods. It provides details on anthropometric measurements like height, weight, and mid-upper arm circumference. It describes clinical signs of nutrient deficiencies and how to check for things like pitting edema. The document also discusses calculating indices from measurements, indicators for malnutrition, measuring muscle mass and fatness, and assessing diets through dietary diversity scores and salt iodine levels.