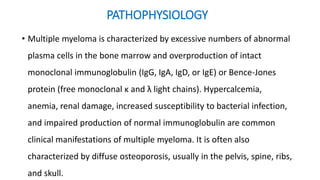
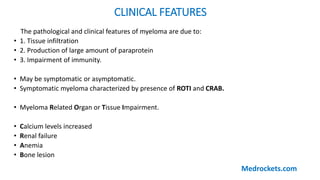
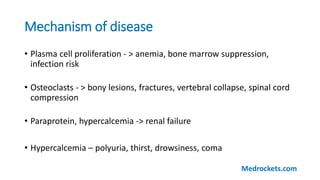
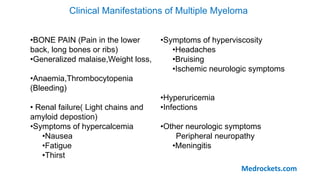
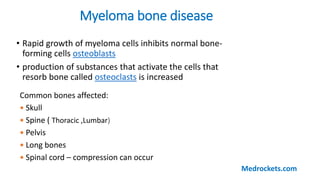
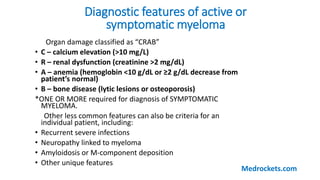
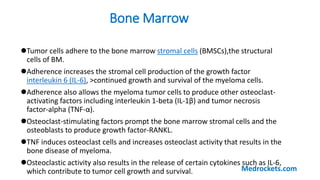
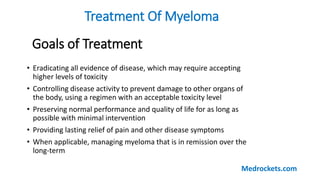
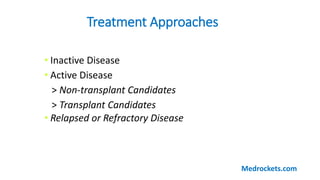
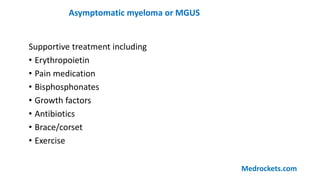
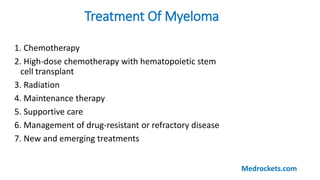
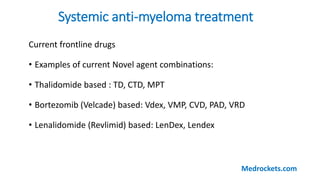
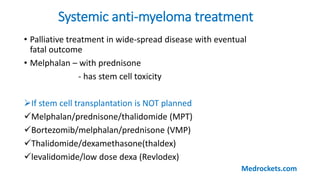
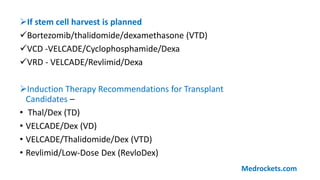
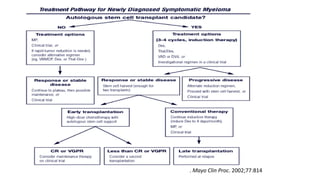
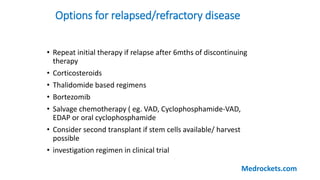
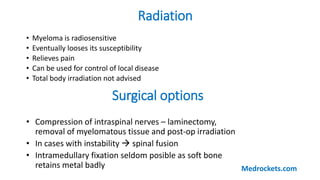
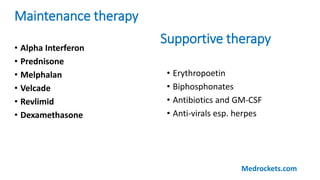
Multiple myeloma is a cancer of plasma cells that are found in the bone marrow. It is characterized by an excessive proliferation of abnormal plasma cells that overproduce a type of antibody known as monoclonal proteins. The disease causes symptoms through tissue infiltration by the plasma cells, overproduction of paraprotein, and impaired immunity. Treatment involves chemotherapy, stem cell transplantation, radiation, supportive care and management of relapsed or refractory disease. The goals are to eradicate the disease, control symptoms, preserve quality of life, and provide long-term remission when possible.