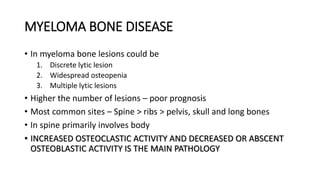
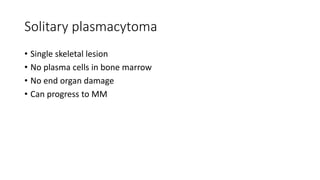
1) Multiple myeloma is a plasma cell neoplasm characterized by monoclonal proliferation of plasma cells that present with skeletal lesions. It most commonly involves the spine, ribs, and pelvis.
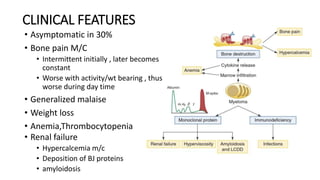
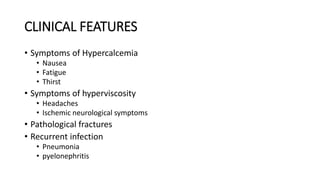
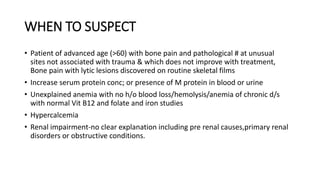
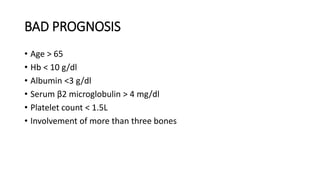
2) Risk factors include age over 60, male sex, and genetic and environmental factors. Presenting symptoms include bone pain, anemia, renal failure, and hypercalcemia.
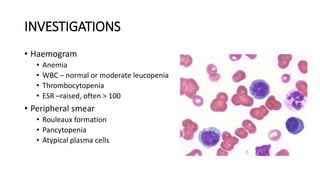
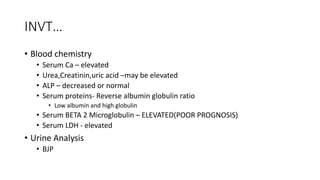
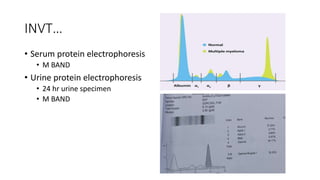
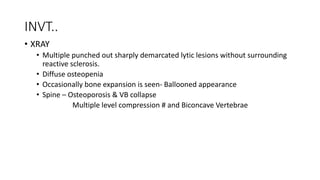
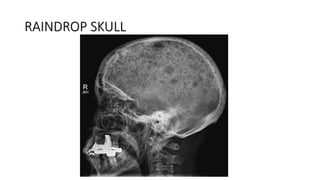
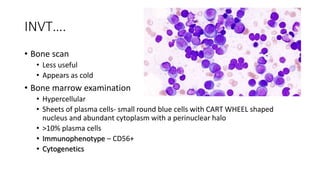
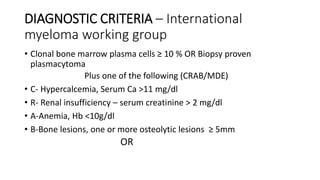
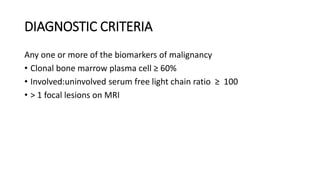
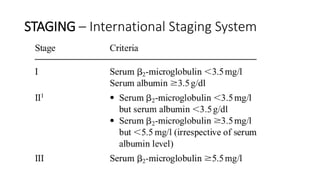
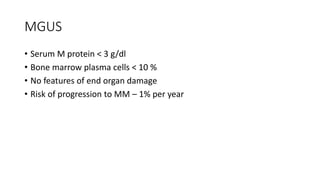
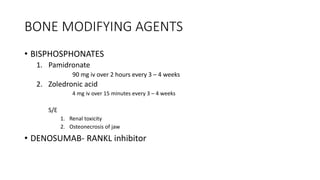
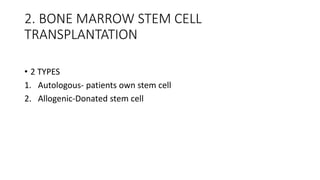
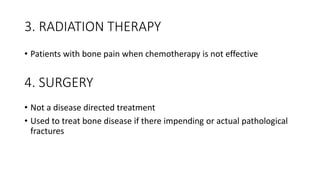
3) Diagnosis involves blood and urine tests showing monoclonal proteins, bone marrow biopsy with over 10% plasma cells, and imaging showing lytic bone lesions. Treatment aims to control the disease and improve quality of life using chemotherapy, steroids, immunotherapy, and stem cell transplantation.