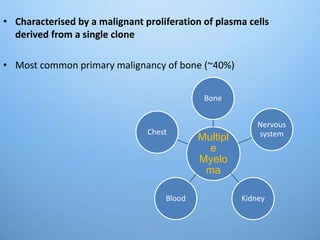
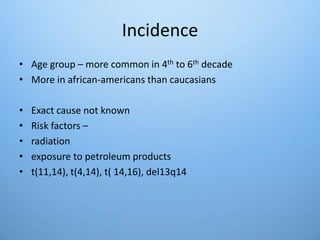
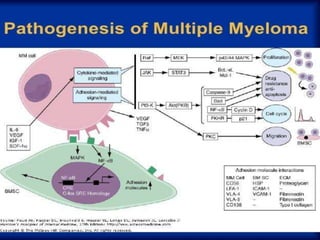
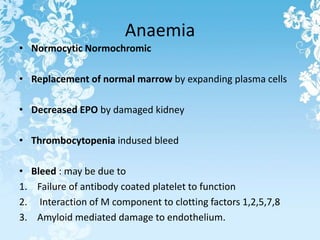
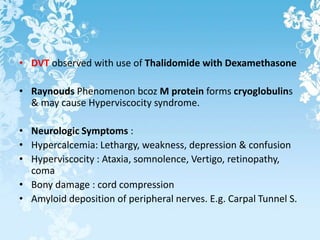
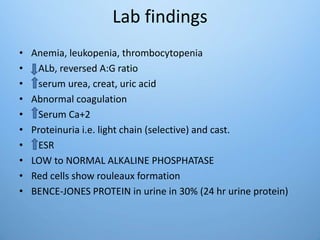
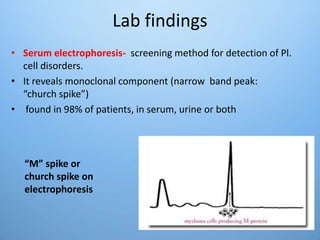
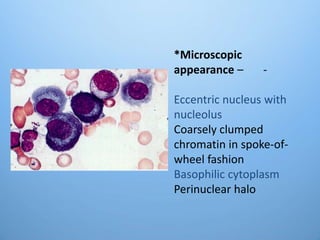
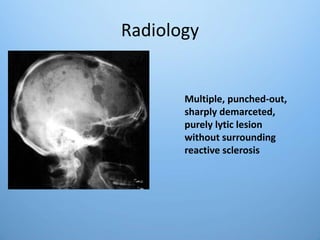
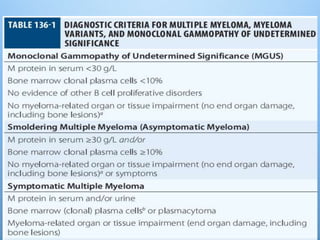
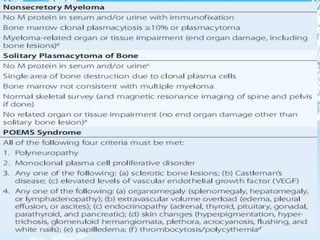
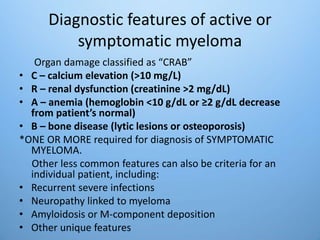
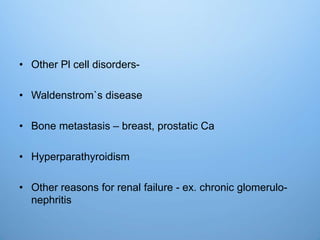
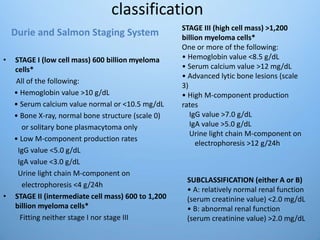
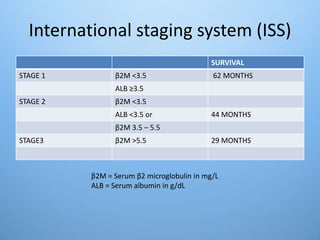
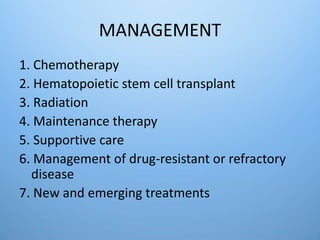
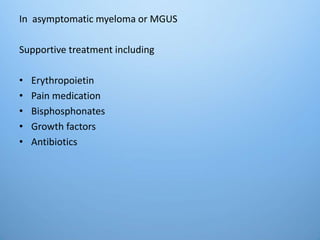
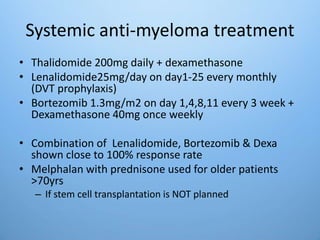
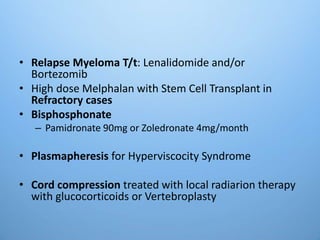
This document provides information about multiple myeloma. It begins by describing multiple myeloma as a malignant proliferation of plasma cells from a single clone that most commonly affects bone. It then discusses the incidence, risk factors, clinical features, recurrent infections, renal failure, anemia, classifications, diagnostic features, laboratory findings, radiology, and management of multiple myeloma. In summary, it provides an overview of multiple myeloma including its causes, symptoms, diagnostic criteria, staging systems, and treatment options.