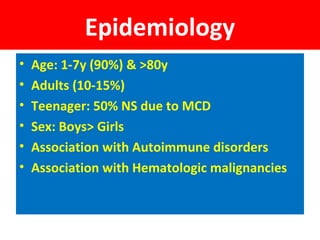
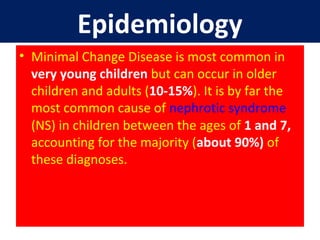
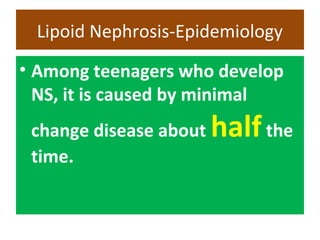
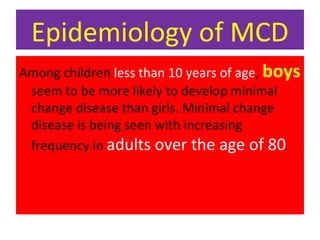
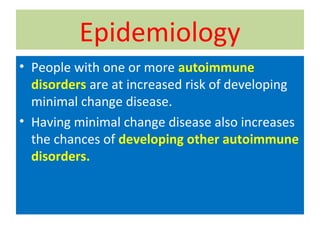
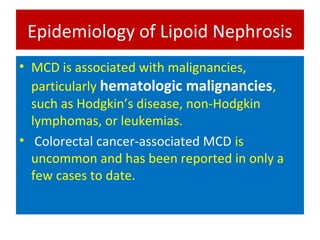
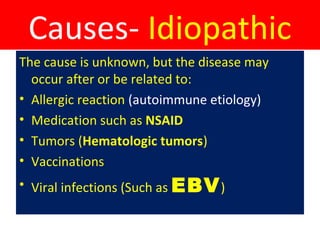
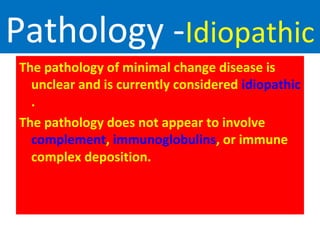
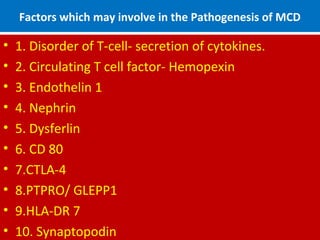
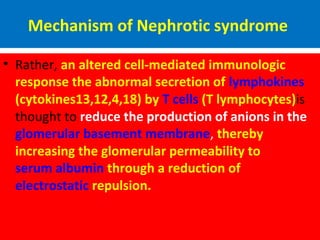
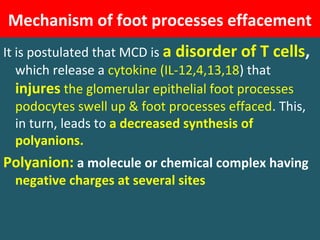
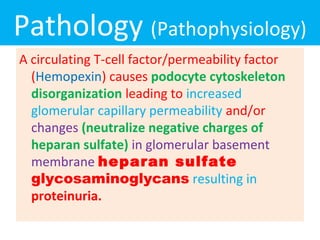
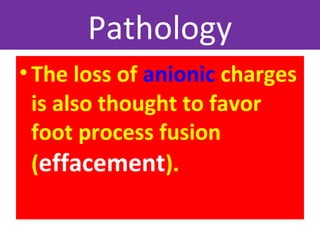
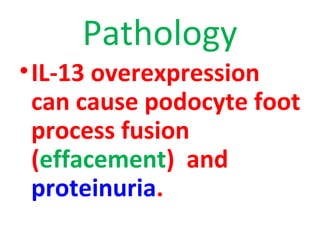
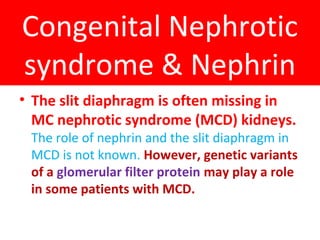
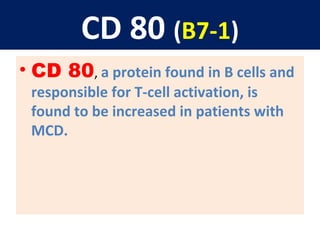
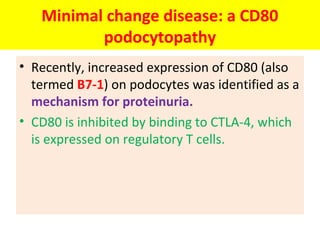
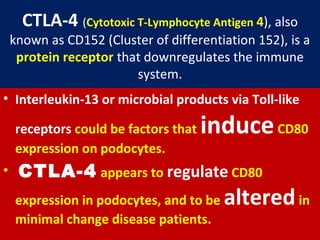
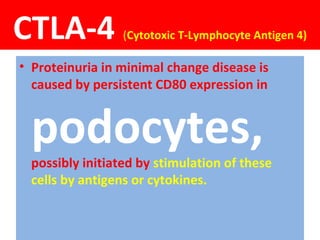
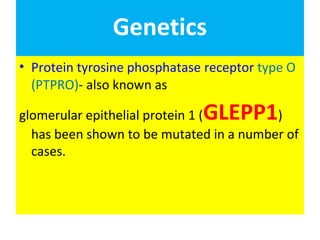
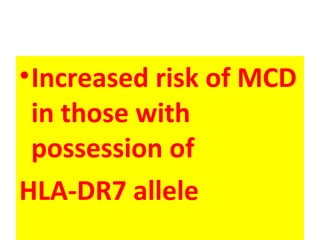
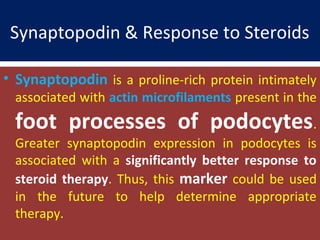
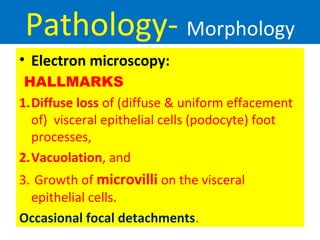
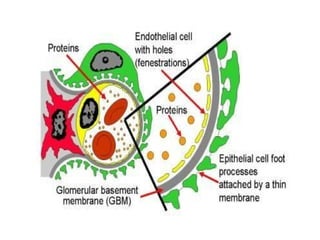
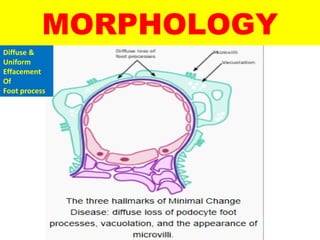
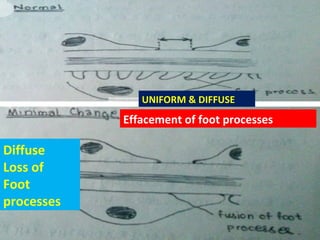
Minimal Change Disease (MCD), also known as Minimal Change Nephropathy, is a kidney disorder characterized by diffuse effacement and loss of foot processes in the glomeruli seen on electron microscopy. It is the most common cause of nephrotic syndrome in children aged 1-7 years and accounts for about 90% of cases. Boys are more commonly affected than girls. MCD is thought to be caused by an abnormal immune response involving T-cells and cytokines that damages the glomerular filtration barrier. This results in proteinuria but no significant pathology on light microscopy. The clinical features include nephrotic syndrome. The prognosis is generally good as over 90% will respond to corticosteroid therapy