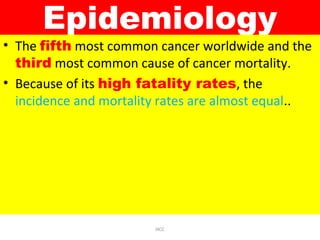
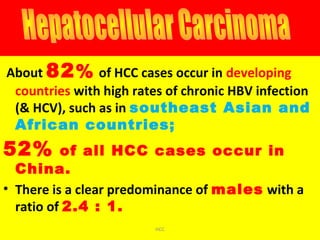
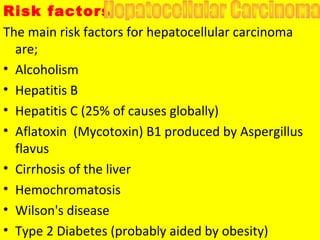
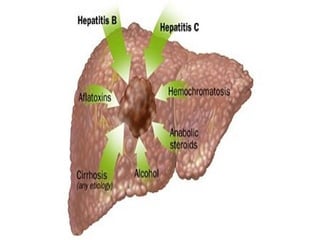
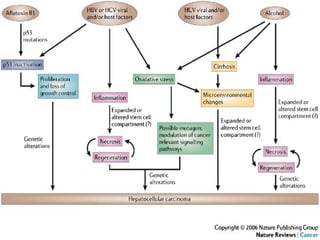
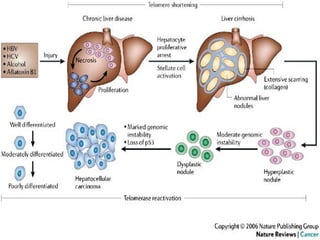
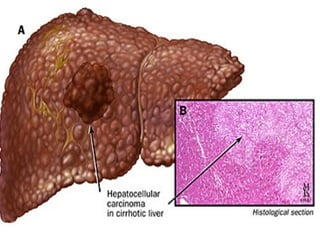
Hepatocellular carcinoma (HCC) is the most common type of liver cancer. It is the fifth most common cancer worldwide and the third leading cause of cancer death. The main risk factors are hepatitis B, hepatitis C, alcoholism, and cirrhosis. HCC often develops from chronic liver inflammation and regeneration caused by these conditions. Patients may present with non-specific symptoms like abdominal pain, weight loss, and fatigue. Diagnosis involves blood tests, imaging studies, and biopsy. Prognosis is generally poor, with most patients dying within 2 years from cancer progression or liver failure.