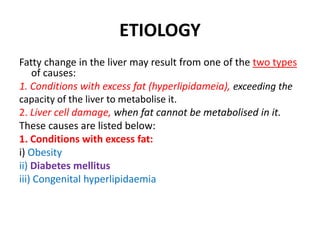
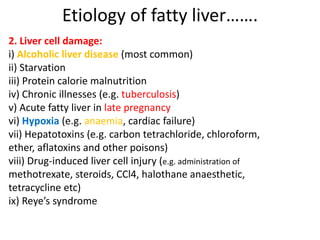
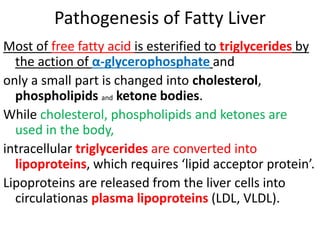
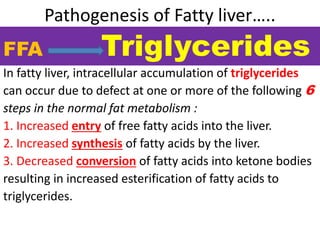
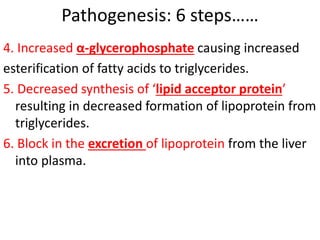
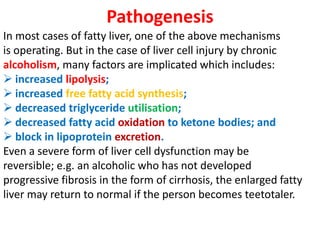
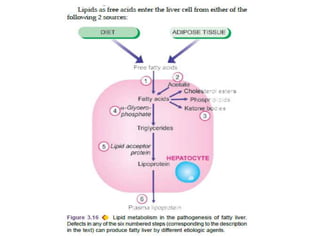
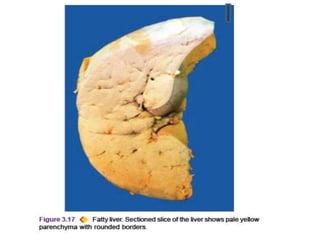
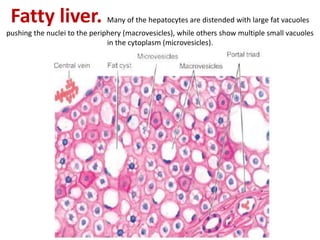
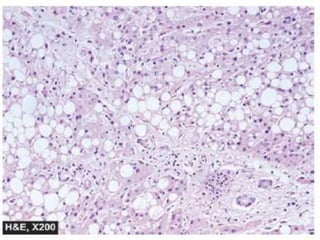
This document discusses fatty change (steatosis) in the liver. It begins by defining fatty change as the intracellular accumulation of neutral fat within parenchymal cells, especially in the liver. It then lists four types of reversible cell injury, including fatty change. The document goes on to discuss the etiology of fatty liver, which can result from excess fat in the body or from liver cell damage. The pathogenesis involves defects in six steps of normal fat metabolism in the liver that lead to triglyceride accumulation. Morphologically, fatty liver is enlarged with a pale yellow appearance. Microscopically, hepatocytes contain numerous lipid vacuoles of varying sizes.