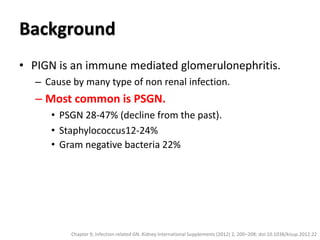
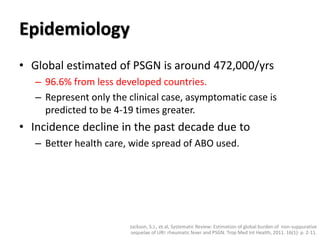
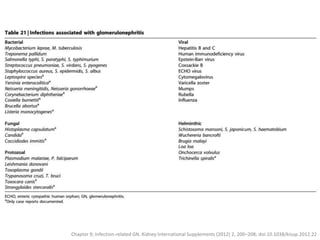
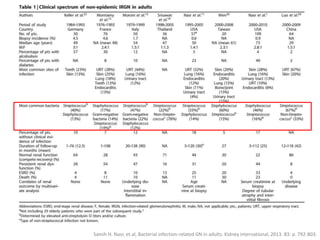
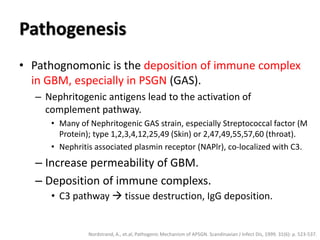
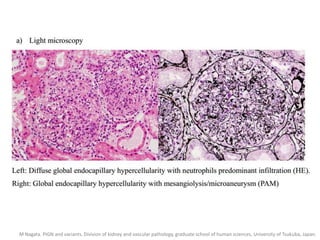
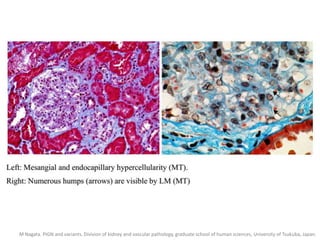
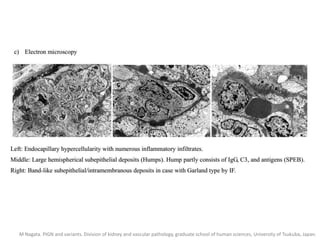
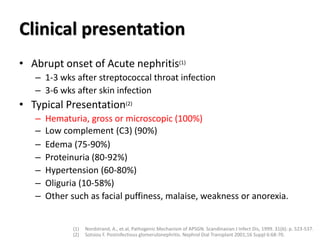
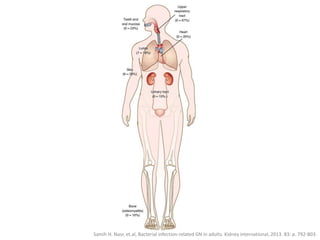
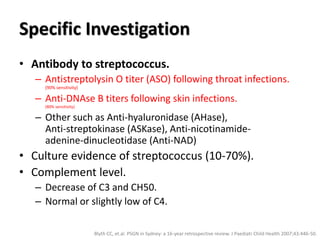
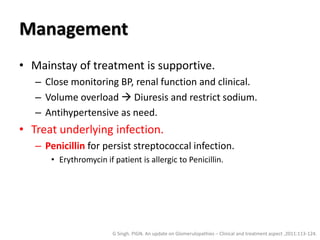
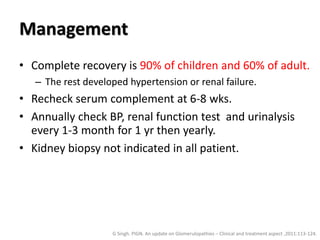
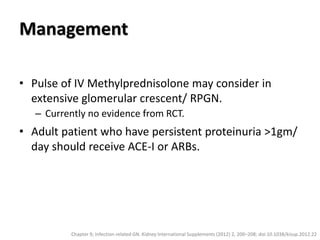
Post Infectious Glomerulonephritis (PIGN) is an immune-mediated glomerulonephritis typically caused by a non-renal infection. The most common cause is Post-Streptococcal Glomerulonephritis (PSGN) following a streptococcal throat or skin infection. PIGN is characterized by the deposition of immune complexes in the glomerular basement membrane. Clinical presentation includes hematuria, proteinuria, edema, and hypertension. Treatment involves supporting the patient and treating any underlying infection. Most patients fully recover, though some may develop long-term complications like chronic kidney disease.