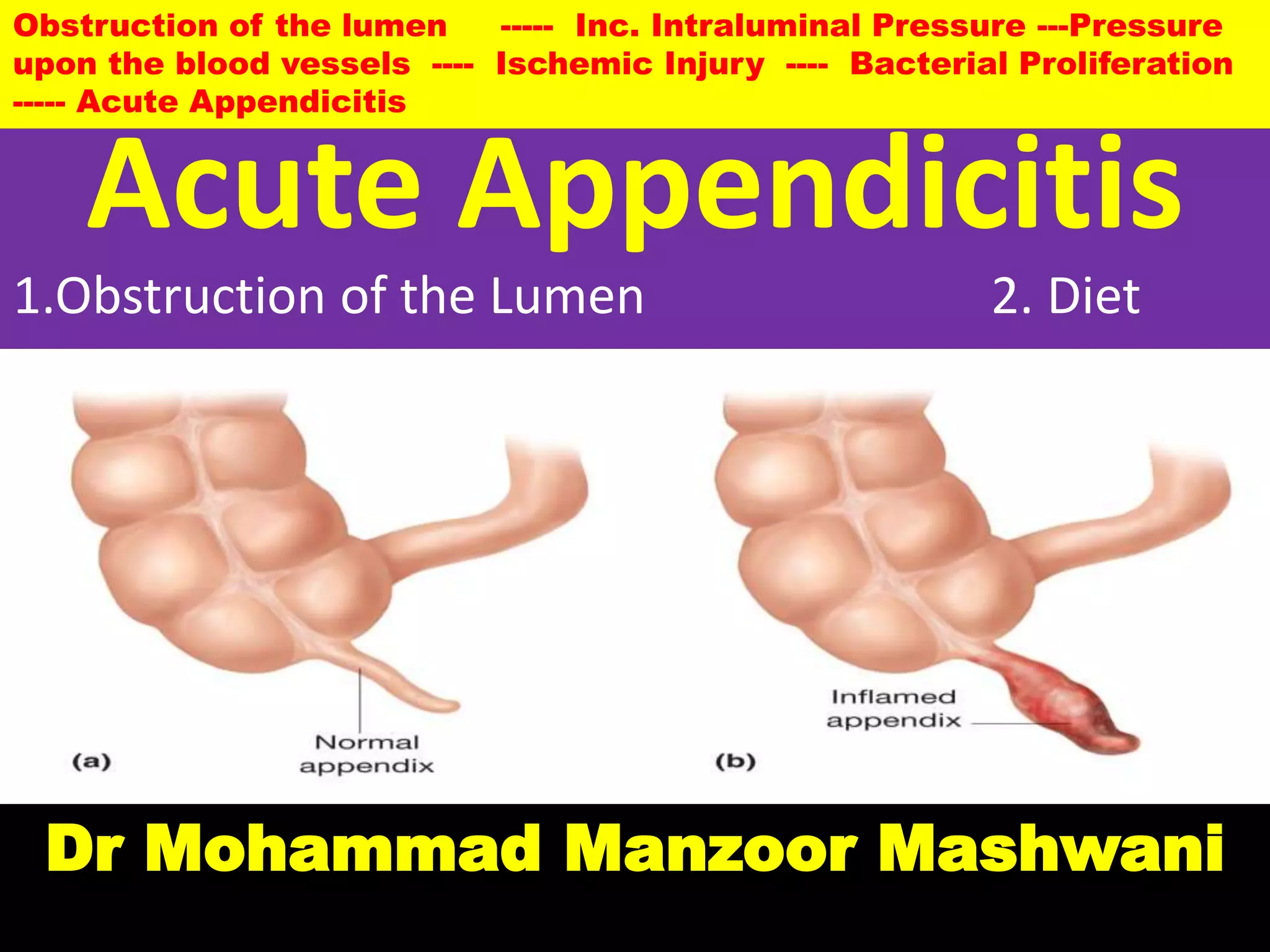
Acute appendicitis is caused by obstruction of the appendix lumen, which increases intraluminal pressure and leads to ischemic injury and bacterial proliferation. On gross examination, early appendicitis shows swelling and redness while advanced cases show necrosis, ulceration and gangrenous changes. Microscopically, early appendicitis is characterized by neutrophilic infiltration of the muscularis propria, while late stages show mucosal sloughing, wall necrosis, and thrombosed vessels. Acute appendicitis is commonly caused by obstruction from fecaliths or lymphoid hyperplasia and presents as abdominal pain.