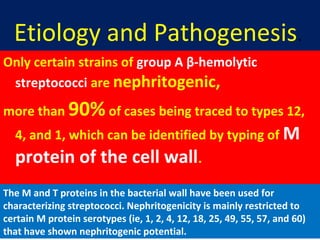
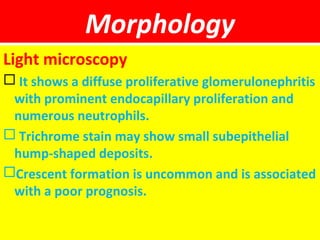
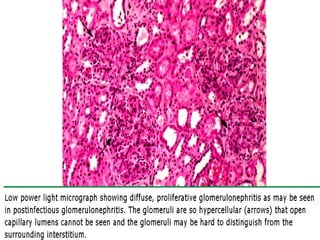
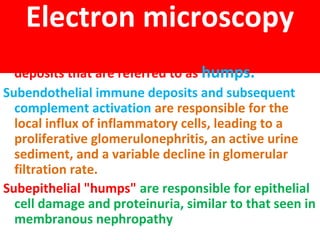
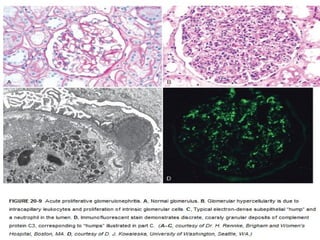
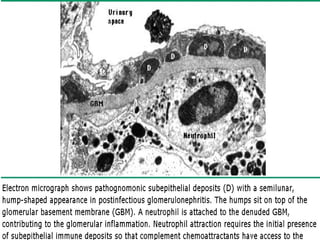
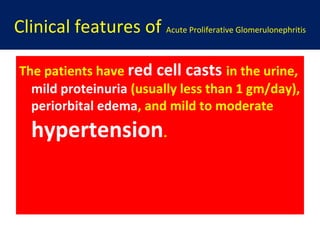
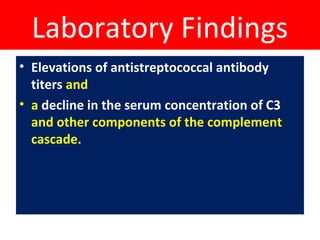
Acute poststreptococcal glomerulonephritis (APSGN) is characterized by sudden edema, hematuria, proteinuria, and hypertension 1-4 weeks after a streptococcal infection. Histologically, there is diffuse proliferation of glomerular cells and leukocytes. It is caused by immune complexes forming in response to certain M protein serotypes of streptococcus. On microscopy, there are subepithelial immune deposits, complement activation, and inflammation, appearing as "humps". Patients typically experience malaise, fever, nausea, and hematuria after a sore throat. Laboratory findings include elevated antibody titers and low complement levels. Most children fully recover with conservative care, while a small percentage progress