The document discusses different types of kidney diseases and disorders:
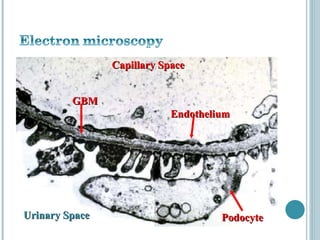
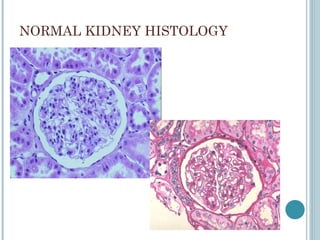
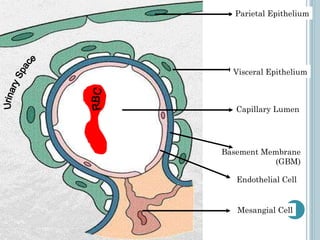
- It describes the normal anatomy and histology of the kidney, including structures like the glomerulus.
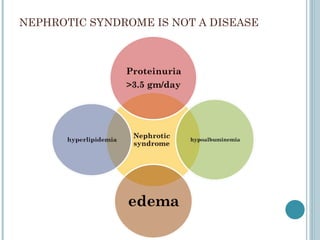
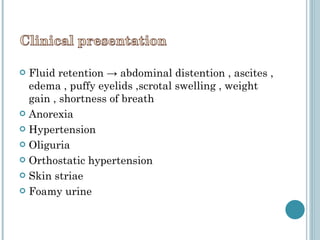
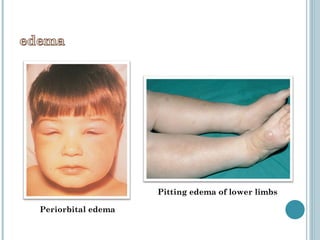
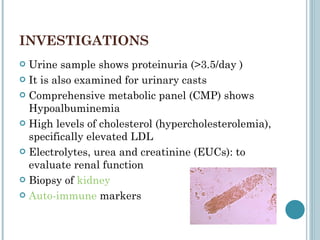
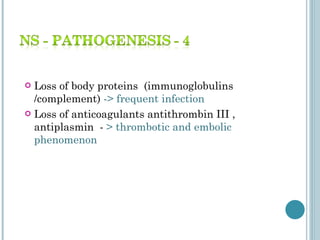
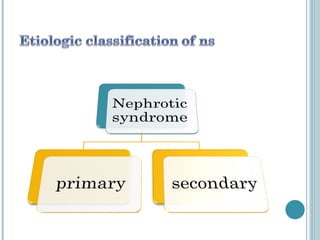
- Nephrotic syndrome is discussed, which is characterized by proteinuria and low albumin levels, causing fluid retention and edema. Investigations include urine tests and kidney biopsies.
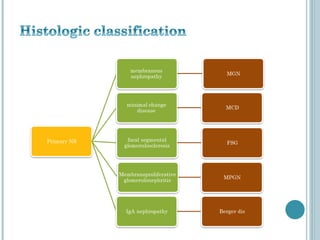
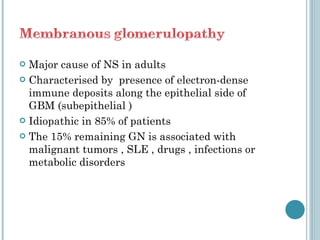
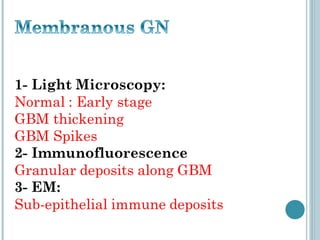
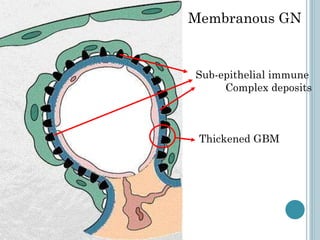
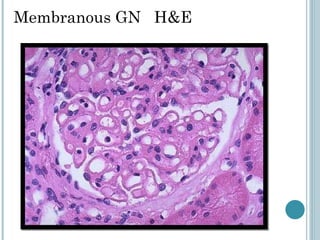
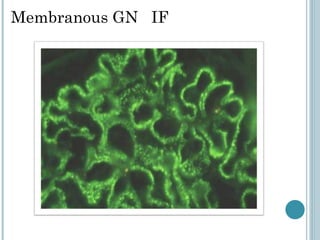
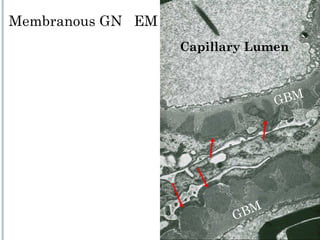
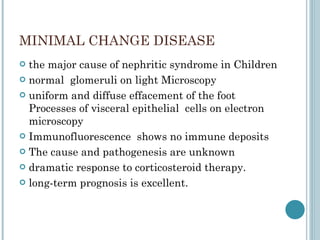
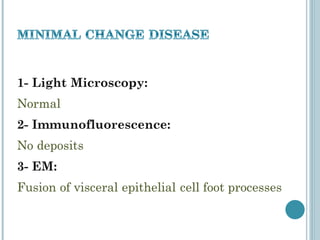
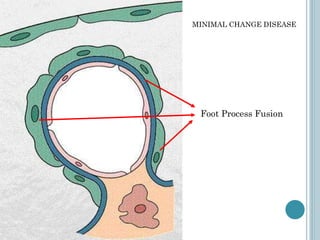
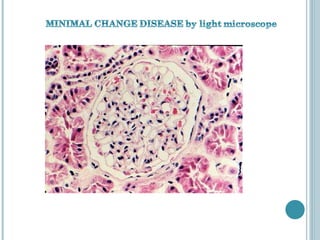
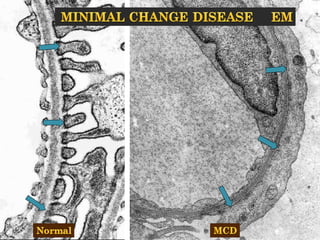
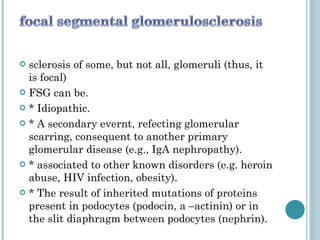
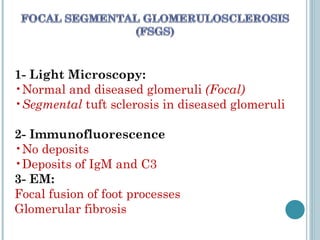
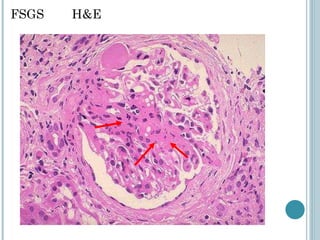
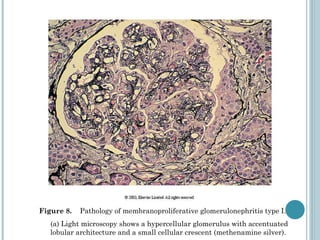
- Different glomerular diseases are described based on their pathology, including membranous glomerulonephritis, minimal change disease, focal segmental glomerulosclerosis (FSGS), and membranoproliferative glomerulonephritis. Their features on light microscopy, immunofluorescence and electron microscopy are provided.
- IgA nep