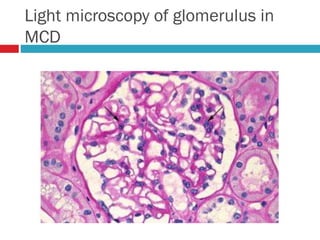
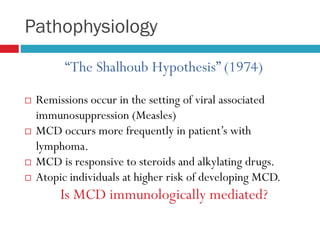
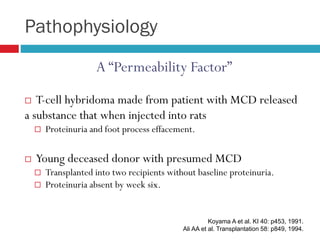
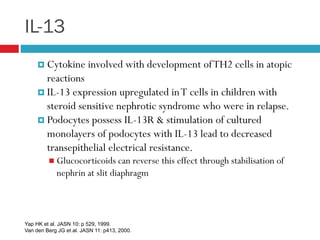
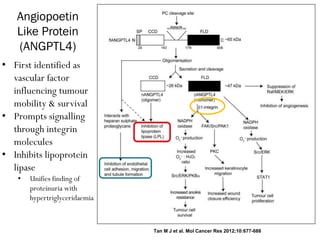
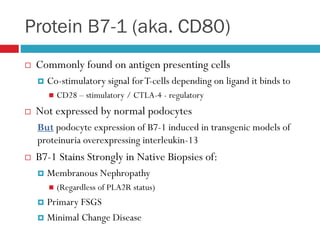
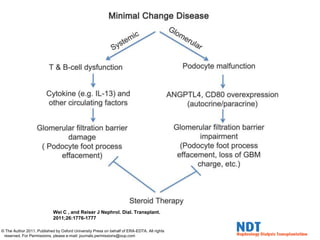
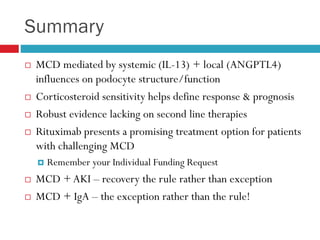
1) Minimal change disease (MCD) is mediated by cytokines like IL-13 and local factors like ANGPTL4 that alter podocyte structure and function, leading to proteinuria.
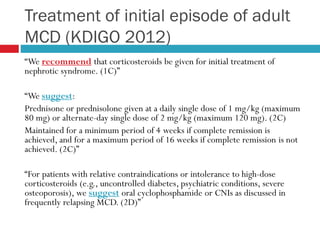
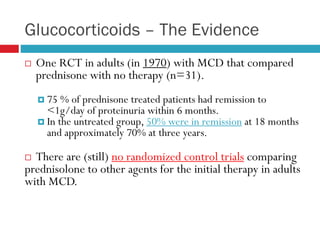
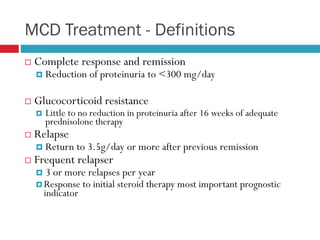
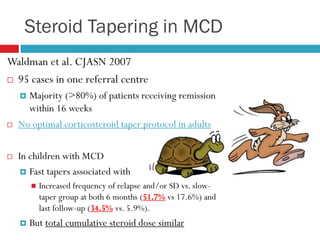
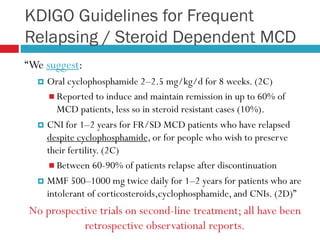
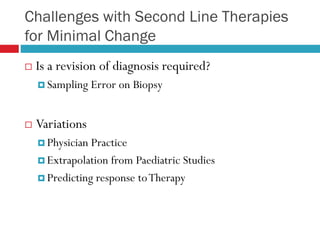
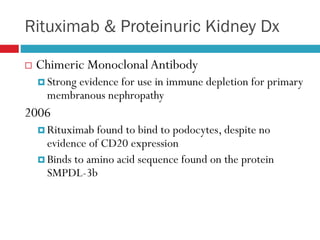
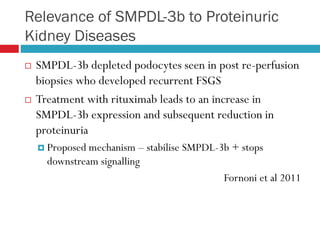
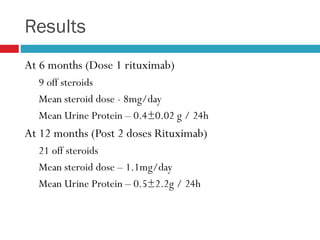
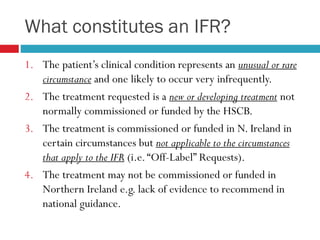
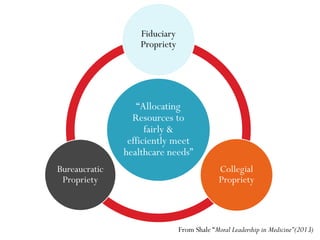
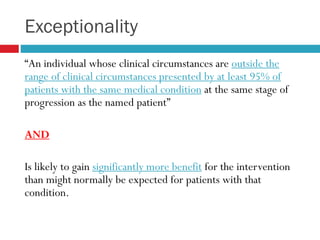
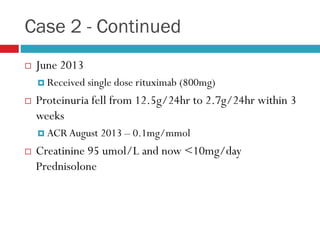
2) Treatment with corticosteroids is usually effective for MCD, but evidence for second-line therapies is limited. Rituximab shows promise but requires approval through an individual funding request process.
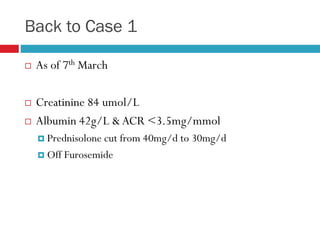
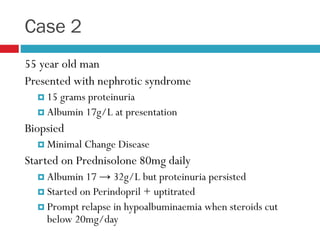
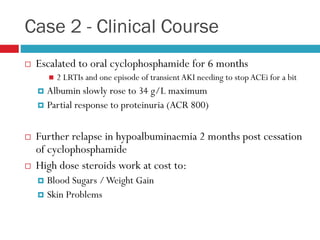
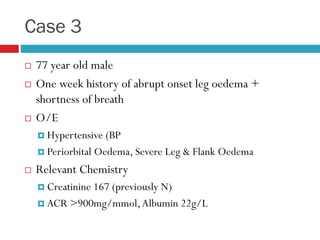
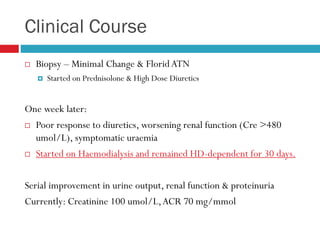
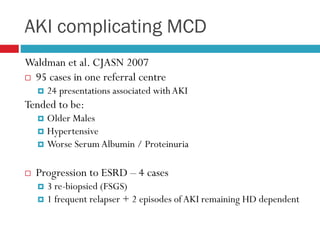
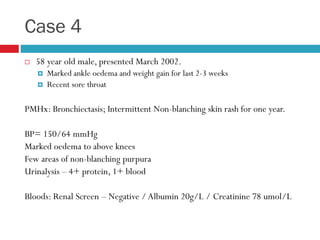
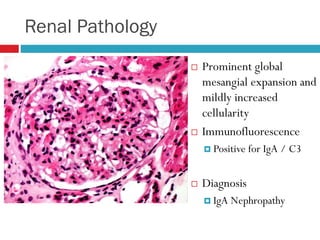
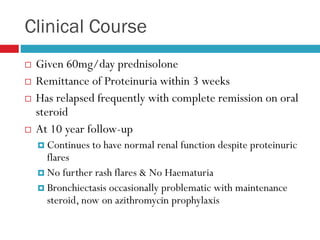
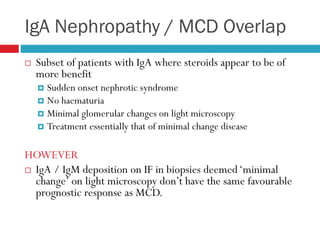
3) While MCD commonly presents as nephrotic syndrome, it can also present as acute kidney injury (AKI) or overlap with other diseases like IgA nephropathy. Recovery is generally good even in complicated cases of MCD.