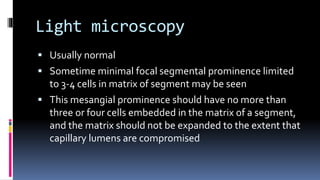
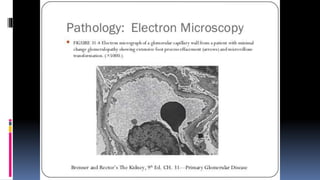
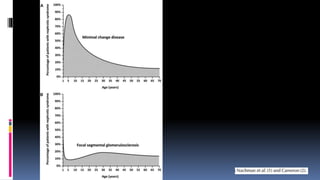
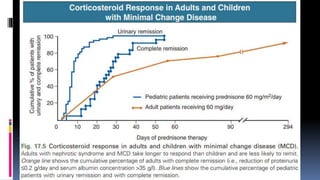
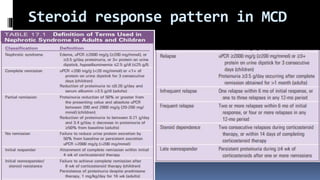
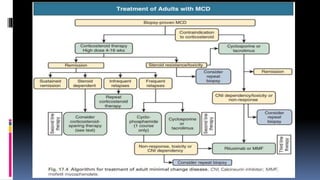
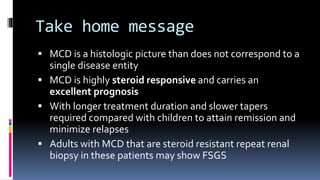
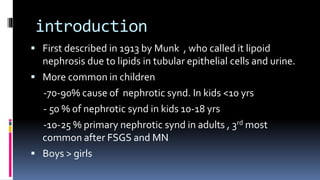
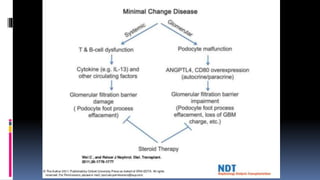
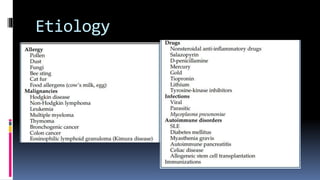
Minimal change disease (MCD) is a histologic pattern seen on kidney biopsy that is characterized by nephrotic syndrome without immune deposits or inflammation. It is most common in children but can occur in adults. The pathogenesis involves circulating permeability factors that cause foot process effacement and proteinuria. MCD is highly responsive to steroids, with remission occurring in 80-85% of adults, though relapses are common. Treatment involves corticosteroids, with slower tapers needed in adults to minimize relapses. Refractory cases may require additional immunosuppression. The prognosis is generally excellent if the disease is steroid-responsive.



![Lab findings
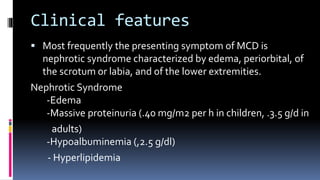
Nephrotic range proteinuria is defined as greater than 3.5
g/24 h
Hypoalbuminemia serum level of albumin below 2.5 g/dl
Hyperlipidemia (elevated total cholesterol and low-density
lipoprotein[LDL] cholesterol)
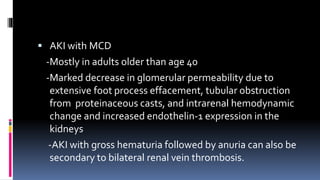
acute kidney injury (AKI) with oliguria secondary to
reduction of intravascular compartment
Mild hyponatremia](https://image.slidesharecdn.com/minimalchangedisease-191217095401/85/Minimal-change-disease-24-320.jpg)