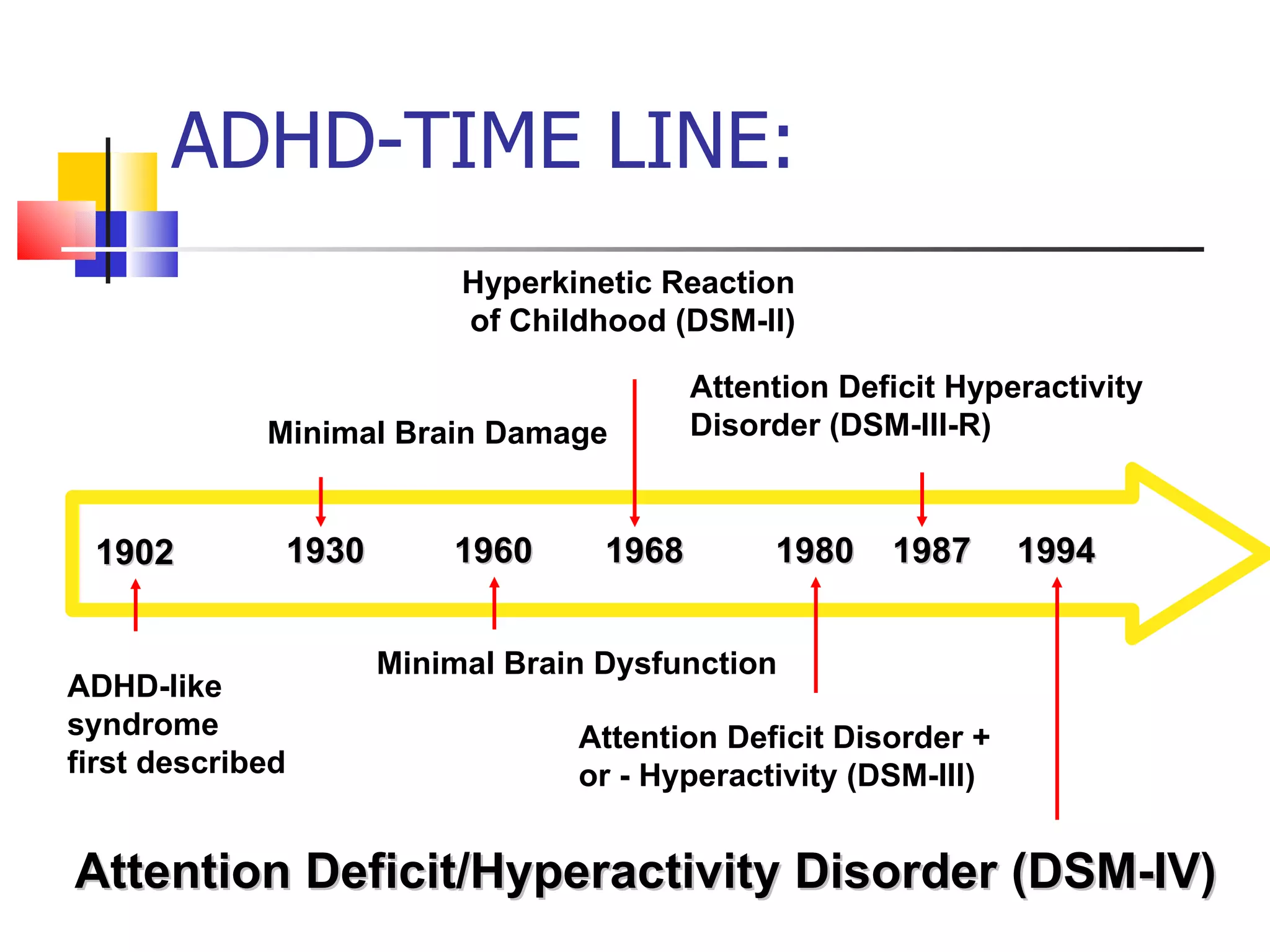
The document discusses attention deficit hyperactivity disorder (ADHD), including:
1) ADHD is characterized by diminished sustained attention and high impulsivity compared to others of the same age. It has three main types and affects 5-10% of the US population, predominantly males.
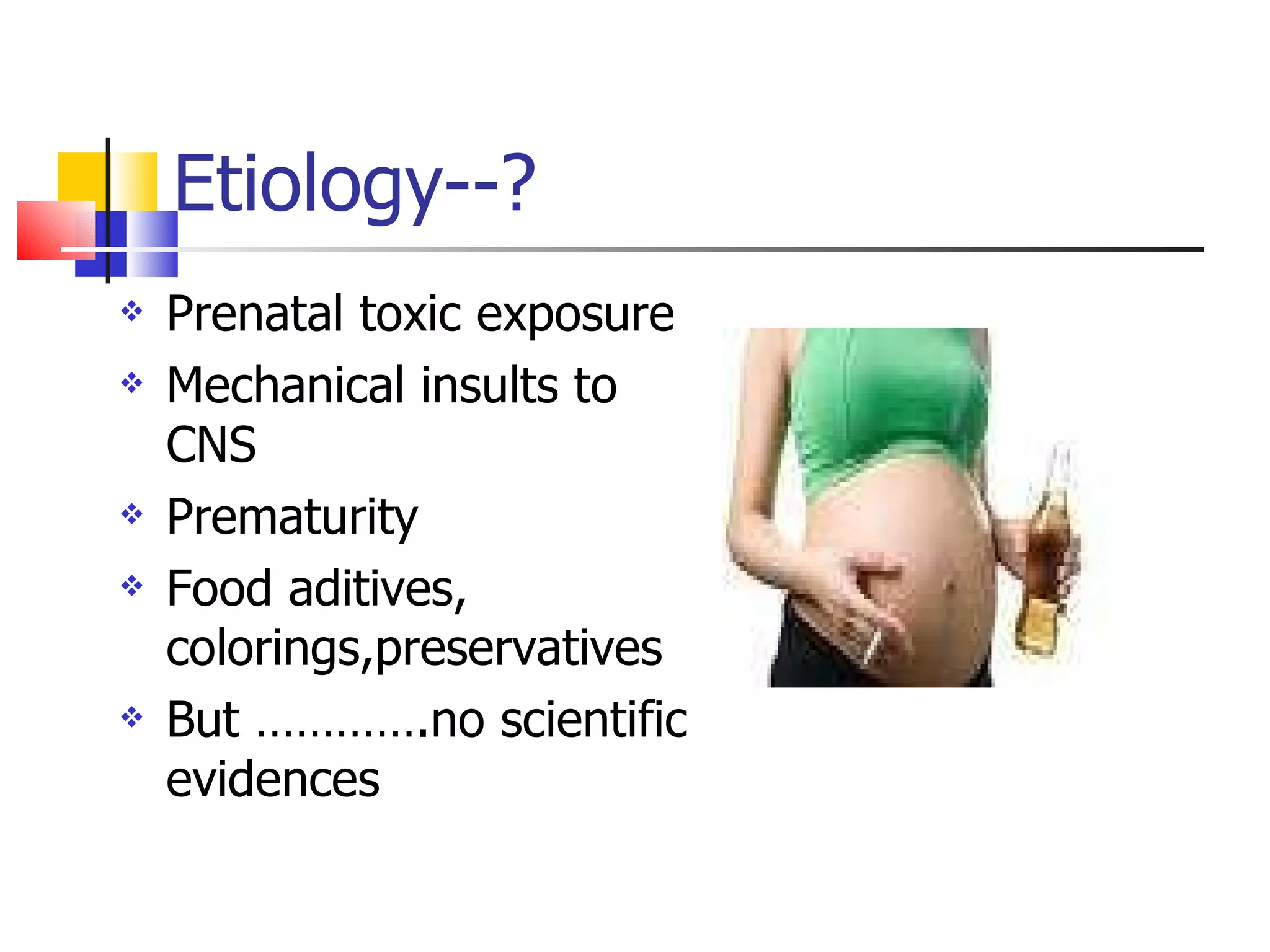
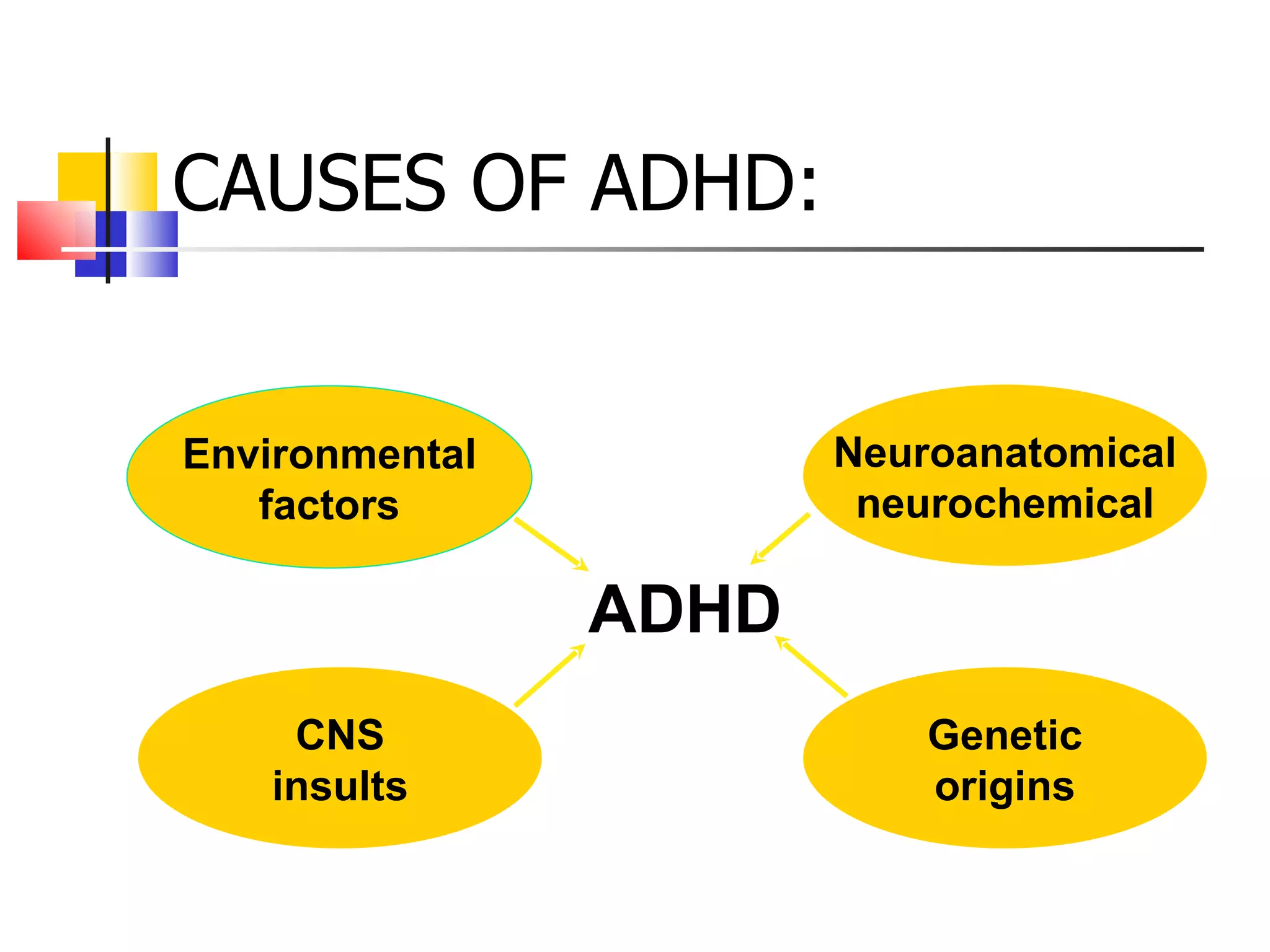
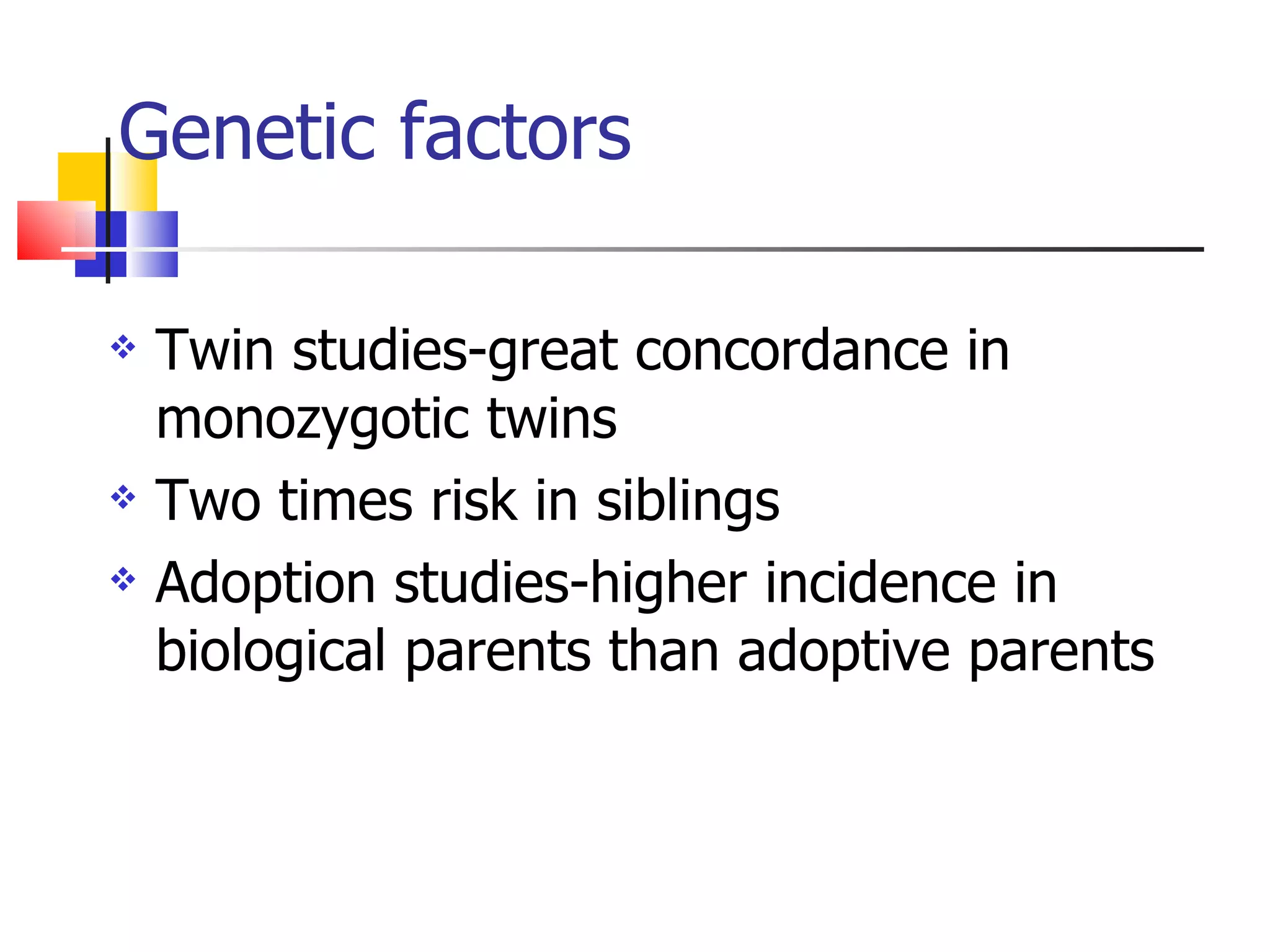
2) ADHD has genetic and neurological causes like central nervous system insults and dysfunction of the noradrenergic and dopamine systems. Stimulant medications are the first-line treatment as they target these systems.
3) Diagnosis involves assessing symptoms, impairment, history, and ruling out other conditions. Treatment includes medication, behavioral modifications, and accommodations at home and school to help manage symptoms.