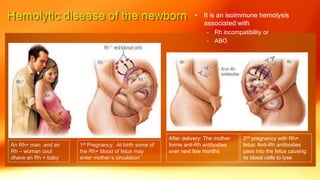
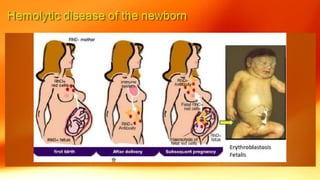
This document discusses neonatal jaundice, including its definition, pathophysiology, types, complications, and management. Key points include:
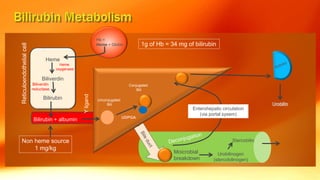
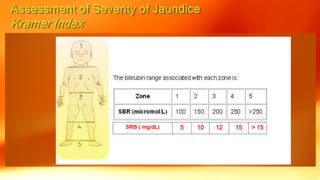
- Jaundice is caused by a buildup of bilirubin, which appears yellow. It is visible in newborns when bilirubin levels reach 5 mg/dL.
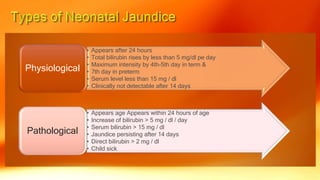
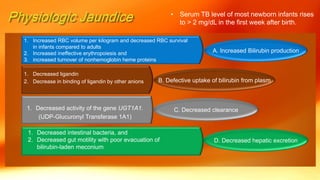
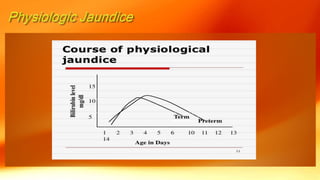
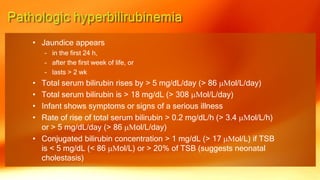
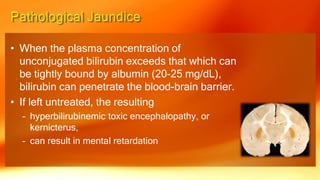
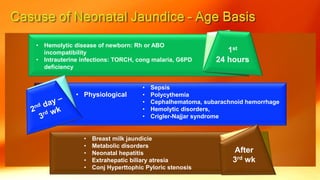
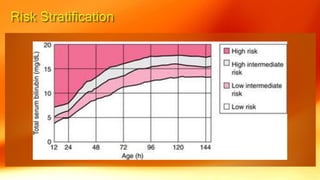
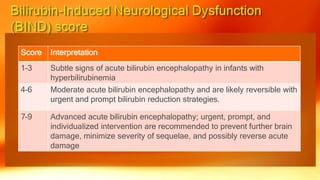
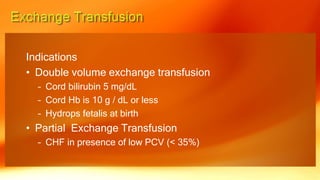
- Physiological jaundice is common in newborns and resolves on its own. Pathological jaundice requires treatment to prevent complications like kernicterus.
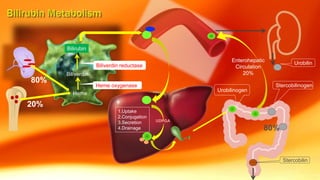
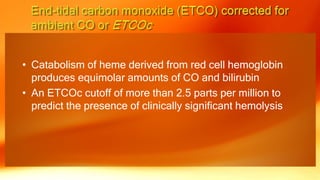
- Causes of neonatal jaundice include an imbalance between bilirubin production and excretion, as well as breastfeeding issues. Treatment depends on the type and severity of jaundice