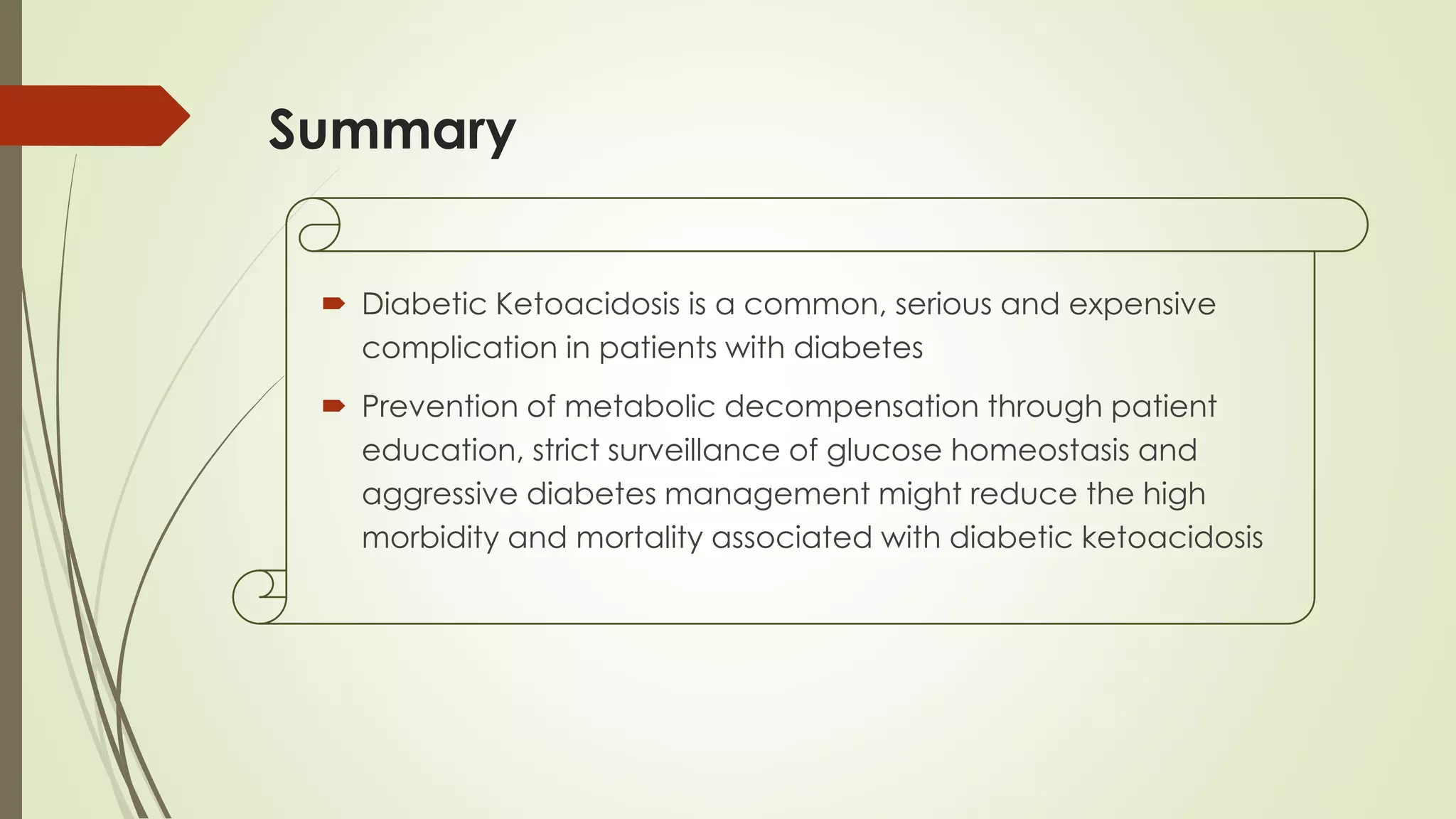
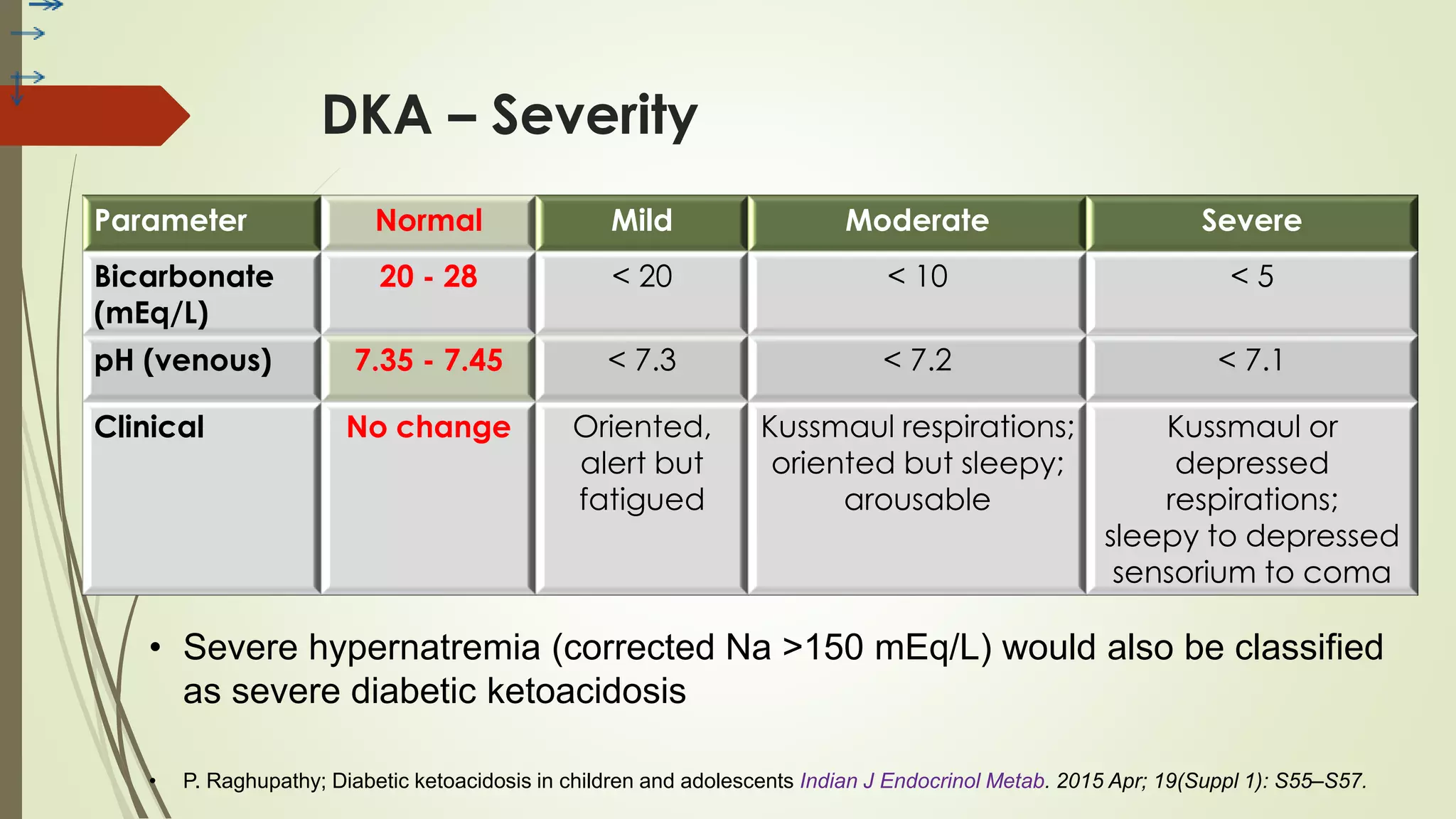
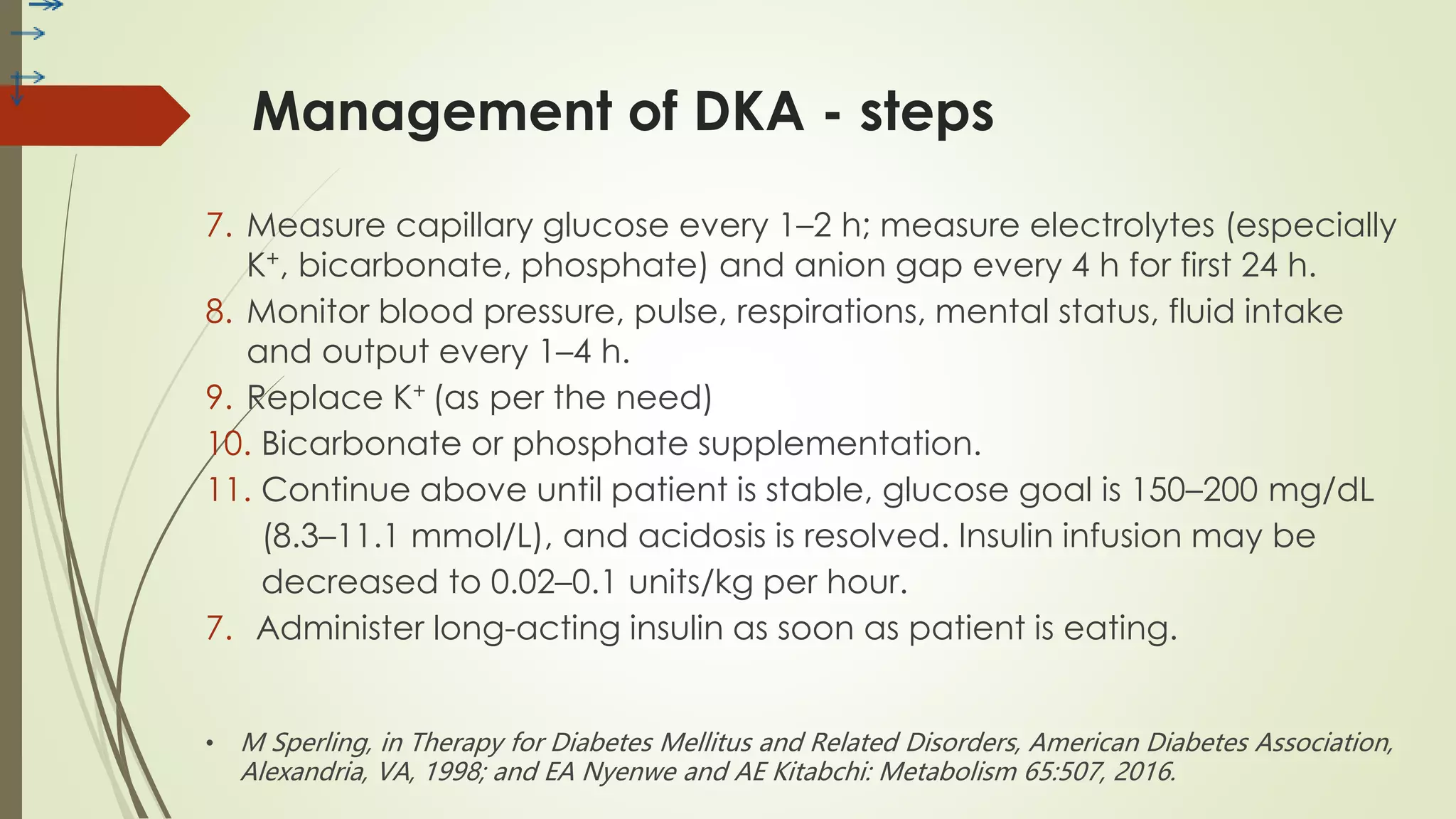
Diabetic ketoacidosis (DKA) is a serious complication of type 1 diabetes, typically triggered by infections, stress, or insufficient insulin. It is characterized by hyperglycemia, metabolic acidosis, and electrolyte imbalances, requiring prompt diagnosis and management including fluid replacement, insulin therapy, and electrolyte monitoring. Effective prevention strategies focus on education and strict glucose monitoring to reduce morbidity and mortality associated with DKA.




















![Treatment of DKA : Sodium replacement
The initial serum sodium is usually normal or low because of the osmolar dilution
of hyperglycemia and the effect of an elevated sodium-free lipid fraction
“True,” serum sodium for any given glucose level above 100 mg/dL (5.6 mmol/L)
is calculated as follows:
[Na+] + (1.6 mEq/L Na+ for every 100 mg/dL glucose in excess of 100)
If the corrected value is > 150 mmol/L, severe hypernatremic dehydration may
be present and may require slower fluid replacement.
Declining sodium may indicate excessive free water accumulation and
increased risk of cerebral edema.
1
2
3
4](https://image.slidesharecdn.com/dkainchildren-200707034836/75/Dibetic-Ketoacidosis-in-Children-23-2048.jpg)