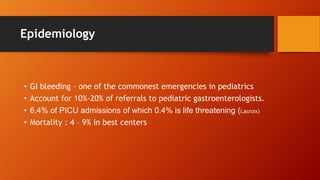
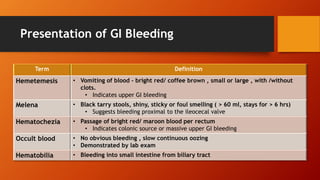
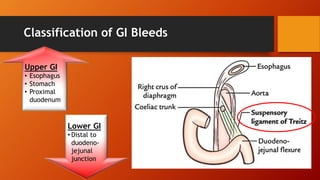
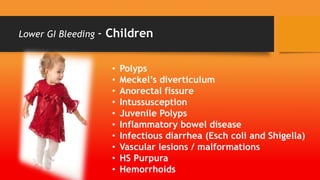
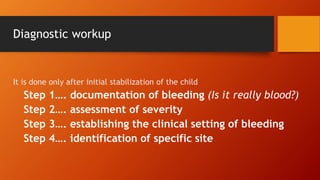
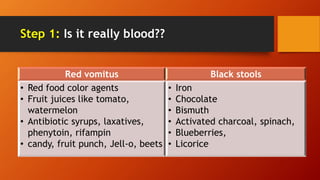
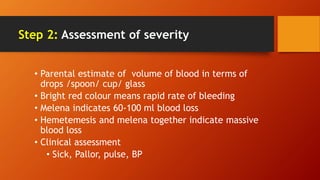
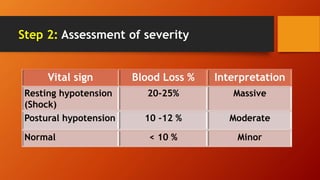
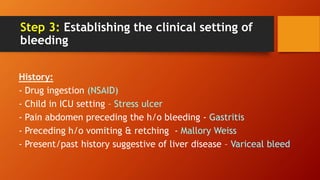
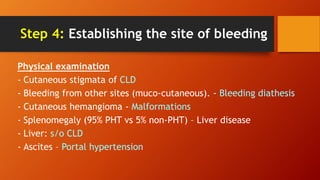
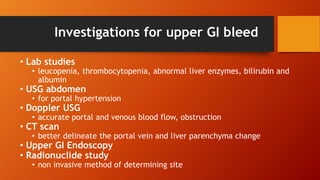
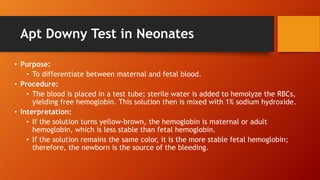
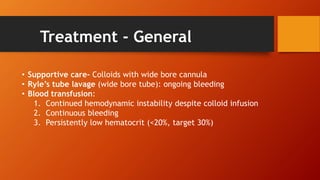
This document discusses gastrointestinal bleeding in children. It notes that GI bleeding accounts for 10-20% of pediatric gastroenterology referrals and around 0.4% of PICU admissions are due to life-threatening GI bleeding. The presentation, classification, causes, diagnostic workup, and treatment of upper and lower GI bleeding in neonates, infants, and children are described in detail over multiple sections. Key points include distinguishing the source and severity of bleeding, identifying specific etiologies, and managing bleeding through supportive care, endoscopic procedures, medications, and surgery as needed.