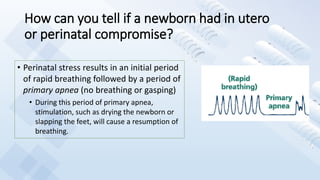
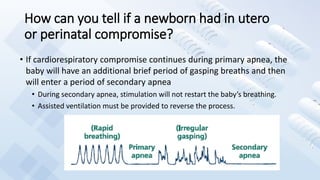
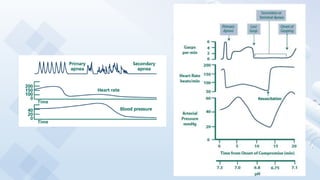
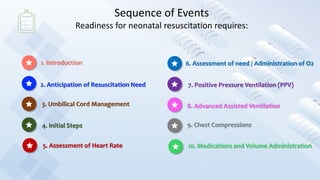
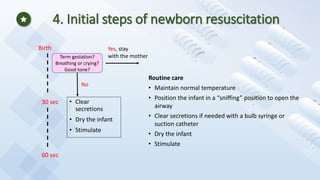
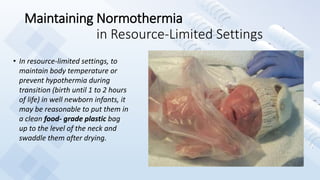
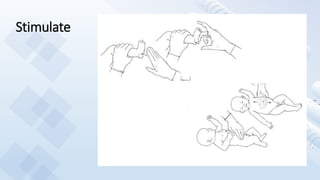
This document provides guidance on newborn resuscitation and delivery room management. It discusses the normal transition from fetal to newborn circulation at birth and signs that can indicate in utero or perinatal compromise requiring resuscitation. It outlines the initial steps of resuscitation including maintaining temperature, positioning, clearing secretions if needed, drying, and stimulating the newborn. It emphasizes timely assessment of heart rate and oxygen need using pulse oximetry to guide ventilation and oxygen administration.


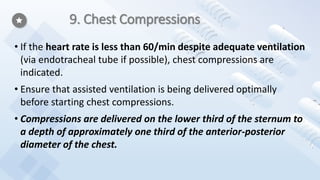
![9. Chest Compressions
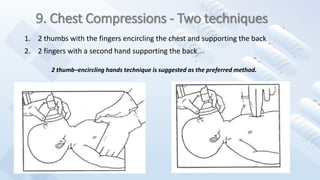
• The chest should be allowed to re-expand fully during relaxation [after each
compression], but the rescuer’s thumbs should not leave the chest.
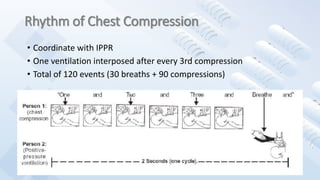
• A 3:1 ratio of compressions to ventilation, with 90 compressions and 30 breaths
to achieve approximately 120 events per minute to maximize ventilation at an
achievable rate is recommended.
• 3:1 compression-to-ventilation ratio is used for neonatal resuscitation where
compromise of gas exchange is nearly always the primary cause of cardiovascular
collapse, but rescuers may consider using higher ratios (eg, 15:2) if the arrest is
believed to be of cardiac origin
• Respirations, heart rate, and oxygenation should be reassessed periodically, and
coordinated chest compressions and ventilations should continue until the
spontaneous heart rate is ≥ 60 per minute.](https://image.slidesharecdn.com/newbornresuscitation-200913083905/85/Newborn-Resuscitation-50-320.jpg)
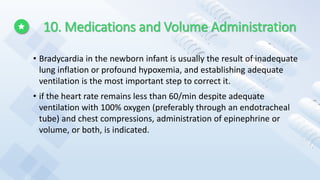
![10.1 Epinephrine
• IV administration of 0.01 to 0.03 mg/kg per dose
is the preferred route [for epinephrine
administration].
• While access is being obtained, administration of a
higher dose (0.05 to 0.1 mg/kg) through the
endotracheal tube may be considered, but the
safety and efficacy of this practice have not been
evaluated.
• Concentration of epinephrine for either route
should be 1:10 000 (0.1 mg/mL).](https://image.slidesharecdn.com/newbornresuscitation-200913083905/85/Newborn-Resuscitation-53-320.jpg)