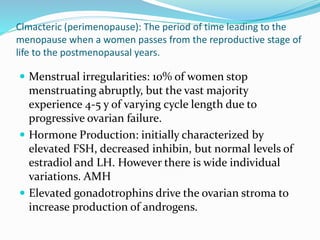
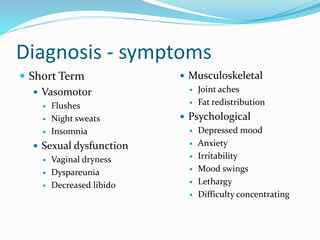
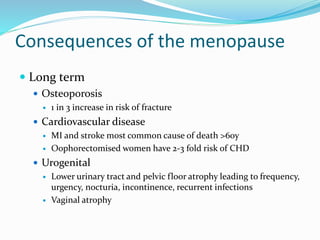
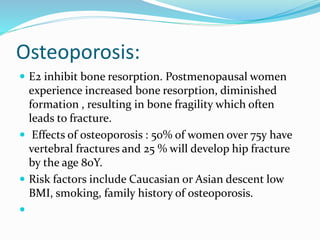
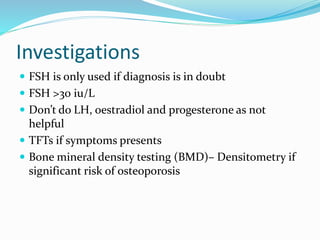
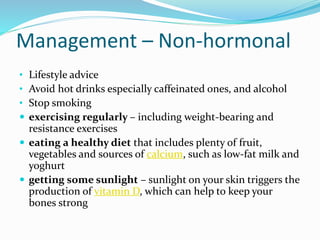
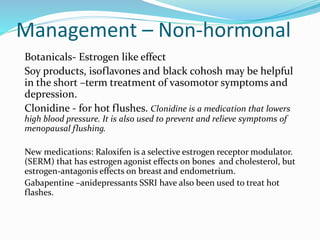
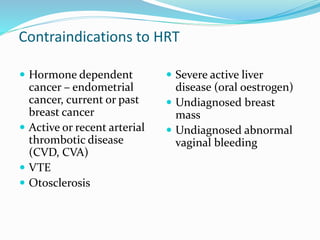
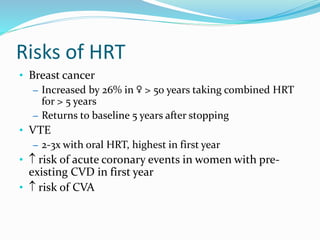
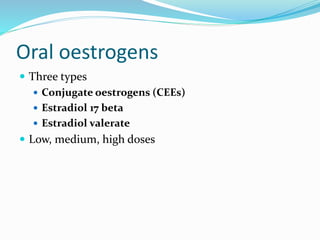
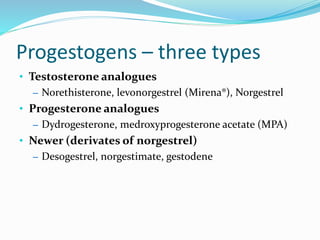
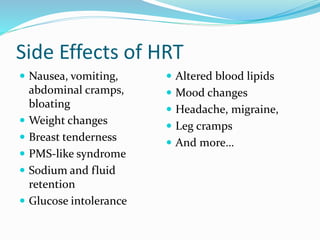
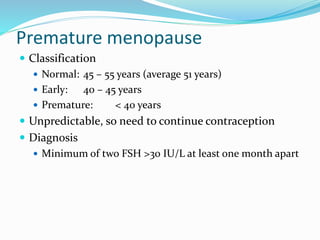
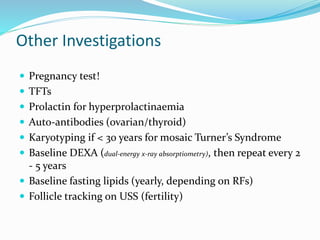
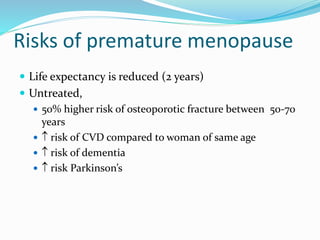
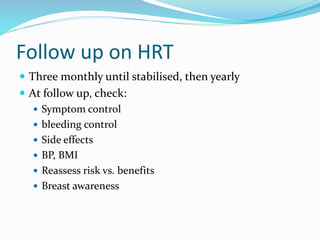
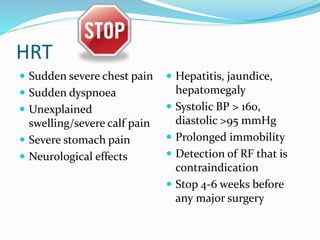
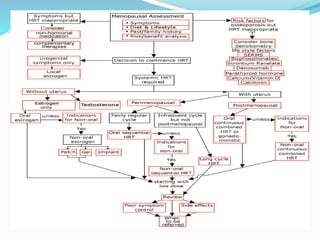
The document discusses menopause, including natural and induced causes. Natural menopause is defined as the permanent cessation of menstruation for 12 months due to ovarian failure. Symptoms include hot flashes, night sweats, and mood changes. Long term risks include osteoporosis and increased risk of cardiovascular disease. Hormone replacement therapy can help treat symptoms and prevent osteoporosis, but has risks like breast cancer if used long term. Lifestyle changes and non-hormonal treatments can also help manage menopause symptoms.