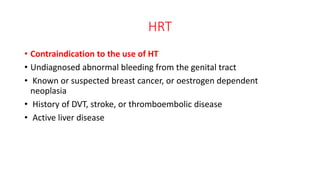
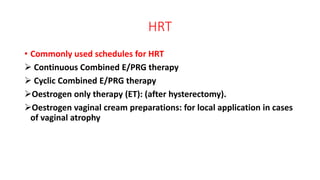
This document discusses menopause, its causes, symptoms, diagnosis, and treatment options. It defines menopause and related terms, and notes that the average age of menopause is around 51 years old. Symptoms can include hot flashes, mood changes, and vaginal dryness. Diagnosis is made if a woman has not had a period in 12 months. Treatment options include lifestyle changes, hormone therapy, and medications to help with symptoms. Hormone therapy has risks but can help treat menopausal symptoms and prevent osteoporosis.