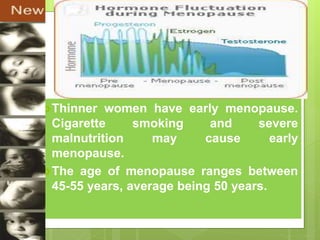
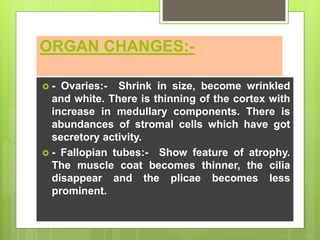
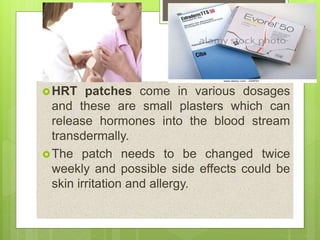
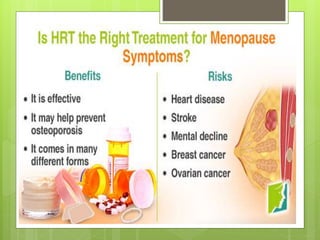
Menopause marks the end of a woman's reproductive years, characterized by a cessation of menstruation for 12 consecutive months due to declining ovarian hormone production. Various stages of menopause include premenopause, perimenopause, and postmenopause, with symptoms such as hot flashes, mood changes, and risks of osteoporosis and cardiovascular disease. Hormone replacement therapy (HRT) is offered to alleviate symptoms, but carries risks that must be carefully managed.