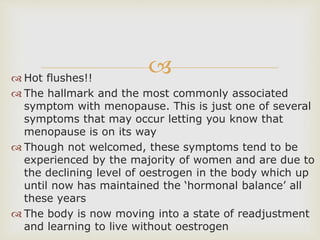
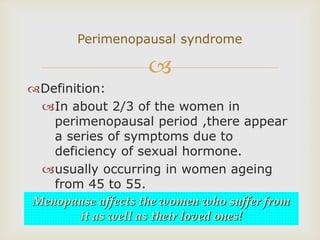
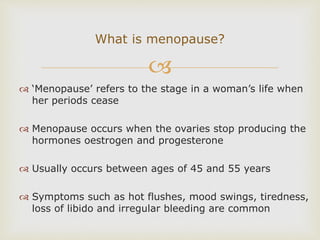
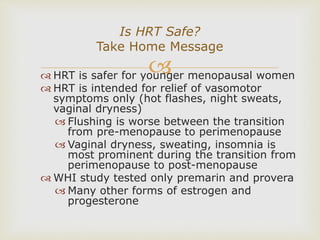
The document outlines the stages and symptoms of menopause, including hot flashes and night sweats, which are common due to declining estrogen levels. It discusses hormone replacement therapy (HRT), its benefits and risks, and emphasizes the importance of lifestyle changes and alternative treatments like Traditional Chinese Medicine for managing menopausal symptoms. The document highlights the need for personalized approaches to effectively address menopause in women.