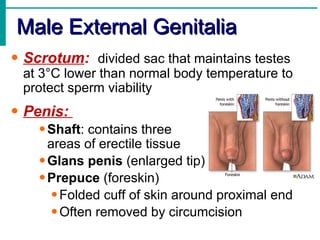
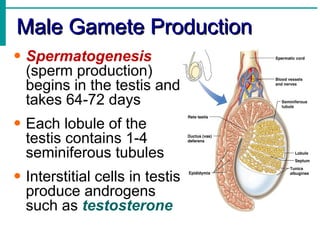
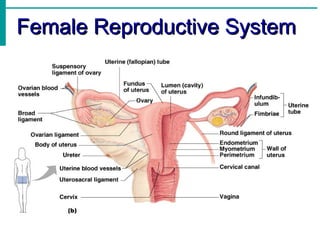
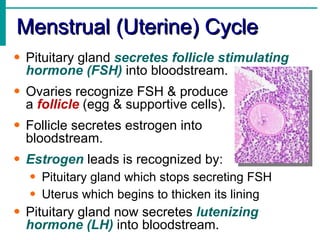
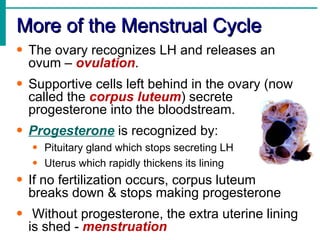
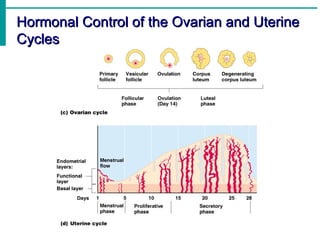
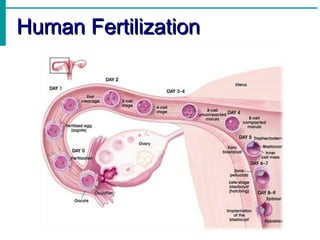
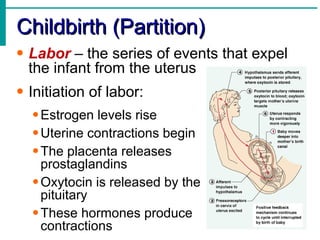
The document provides an overview of the human reproductive system, including its anatomy, physiology, development and functions. It describes the key structures and roles of the male and female reproductive systems, from gamete production and fertilization to childbirth. Key topics covered include the gonads, hormones, menstrual cycle, sexual reproduction and development from fertilization through the embryonic stages.