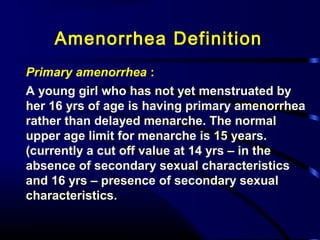
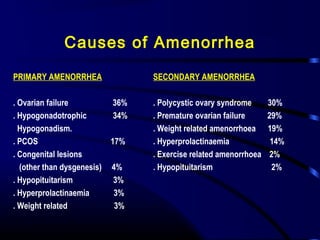
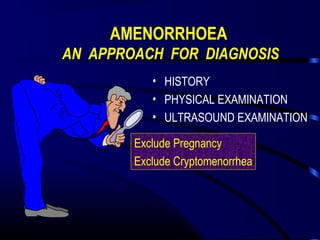
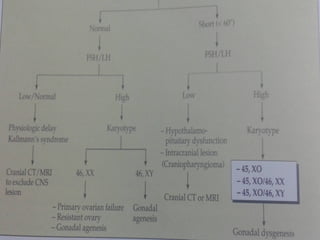
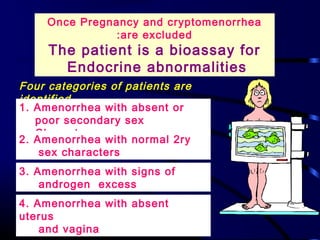
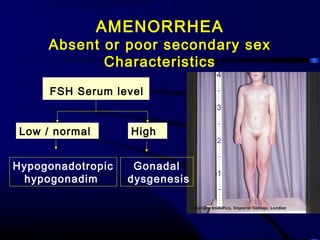
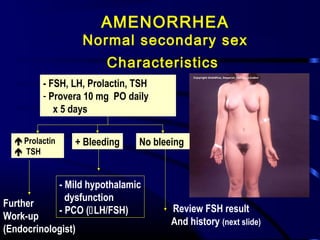
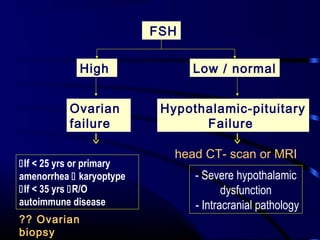
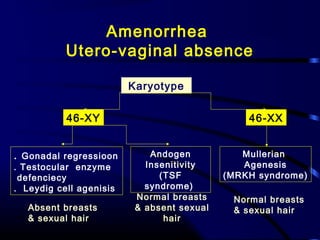
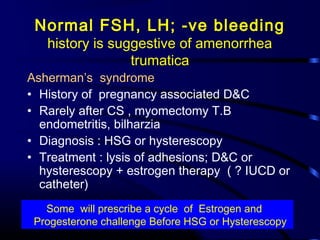
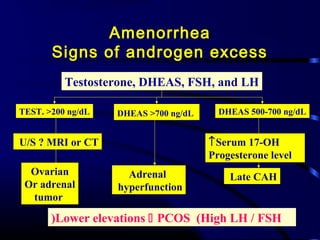
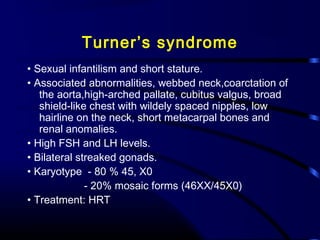
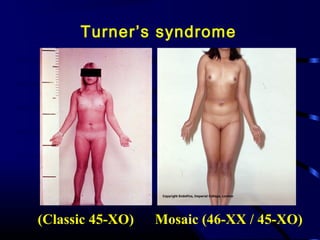
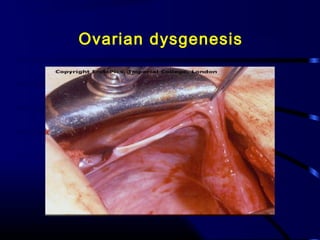
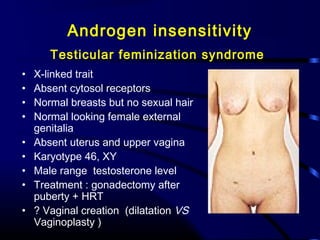
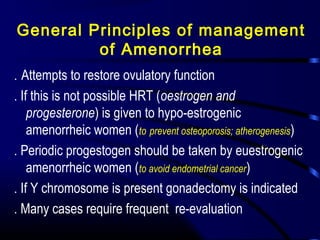
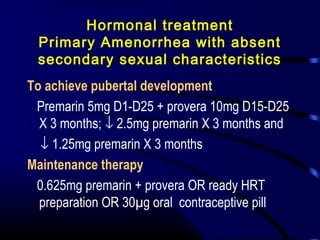
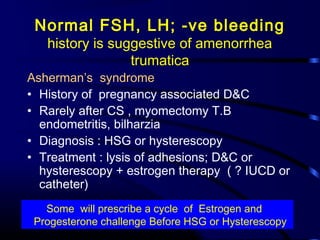
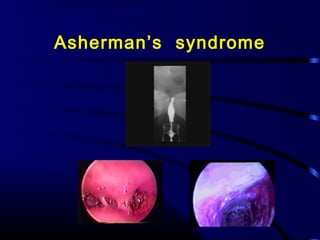
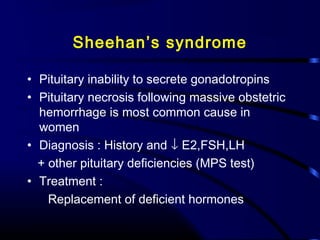
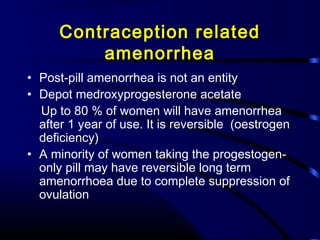
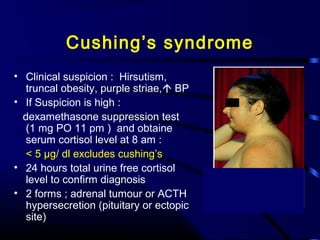
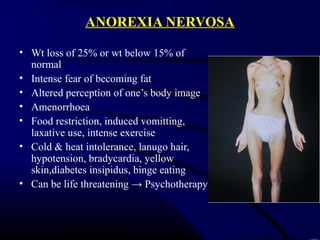
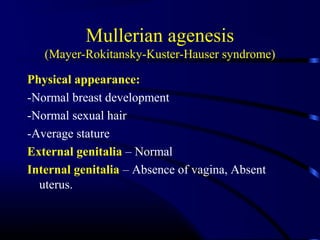
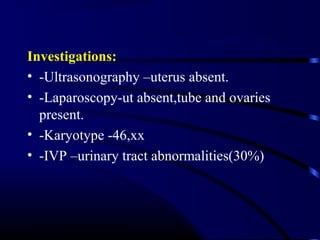
The document discusses amenorrhea, its classification, causes, diagnosis and management. It defines primary amenorrhea as the absence of menstruation by age 16 and secondary amenorrhea as absence of periods for 3 months in a previously menstruating woman. The main causes outlined include hypogonadotropic hypogonadism, polycystic ovary syndrome, premature ovarian failure, hyperprolactinemia, and weight-related issues. The diagnostic approach involves assessing the history, physical exam, ultrasound and hormonal levels. Management focuses on restoring ovulation if possible, or replacing hormones as needed to prevent health issues.