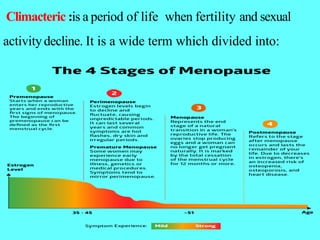
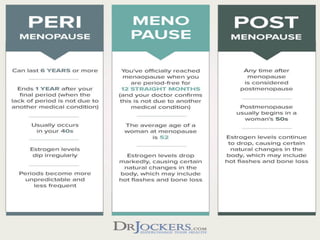
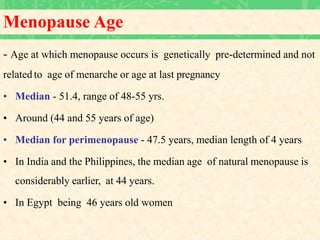
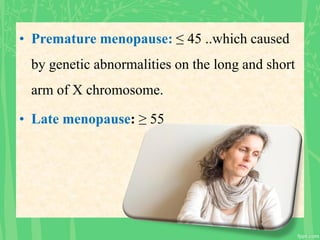
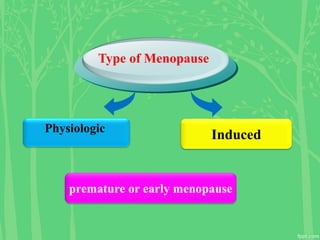
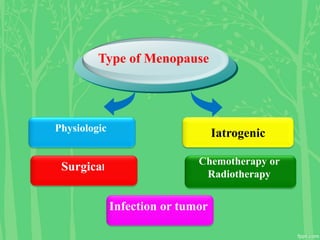
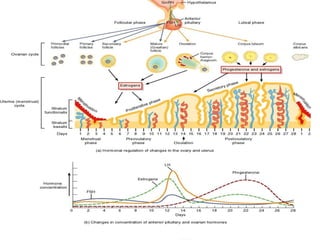
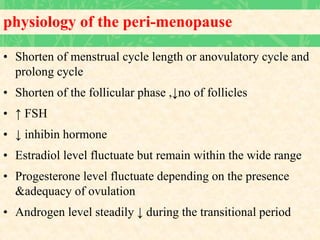
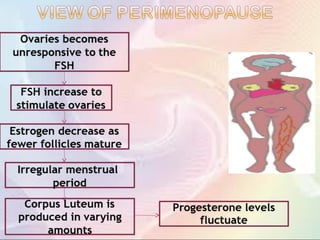
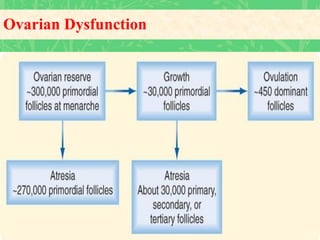
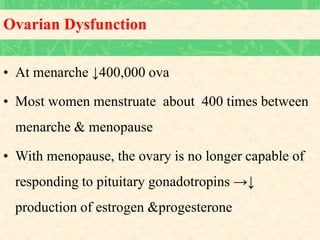
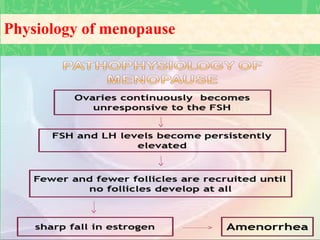
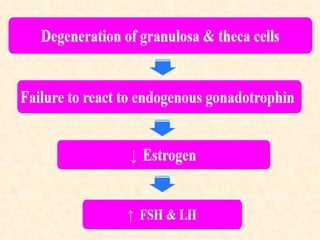
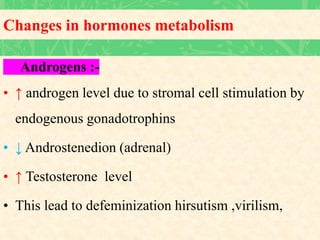
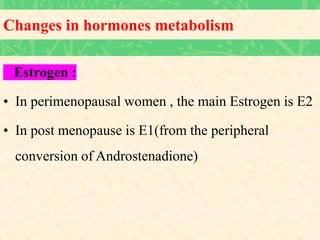
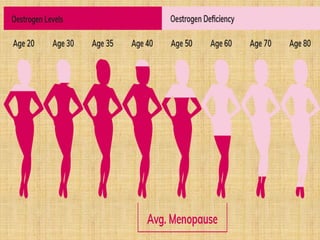
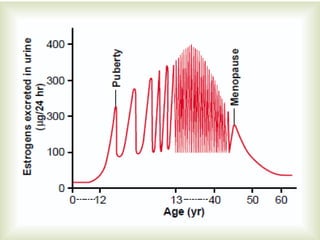
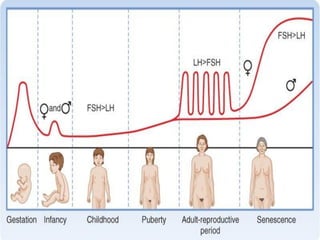
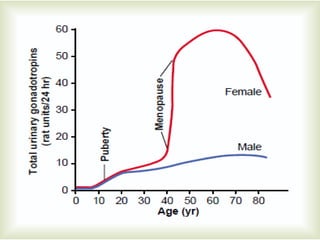
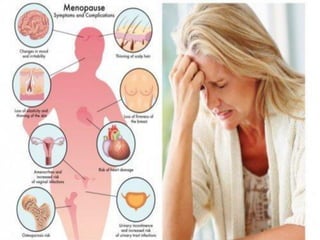
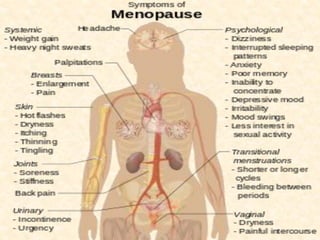
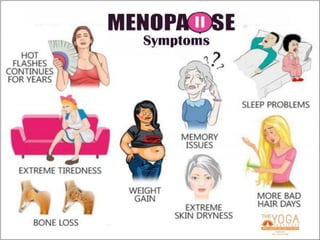
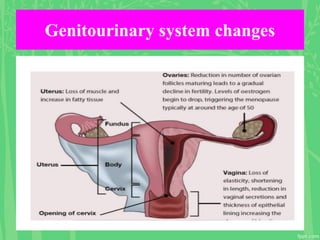
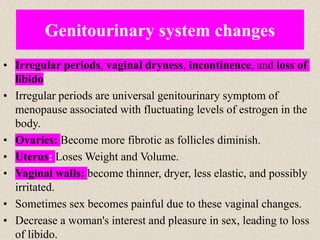
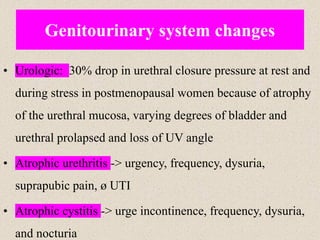
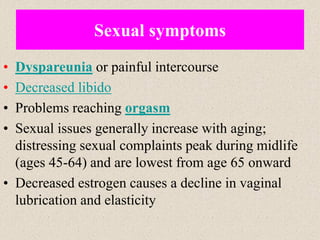
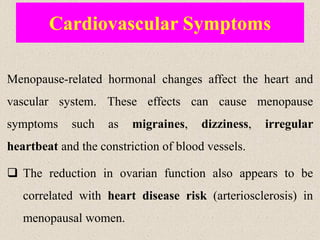
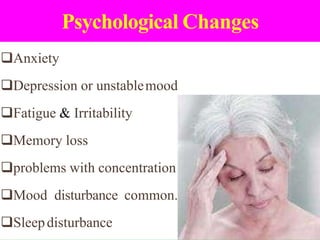
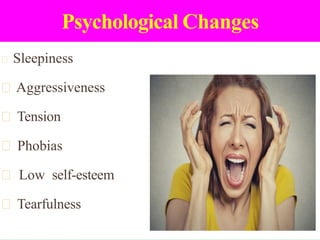
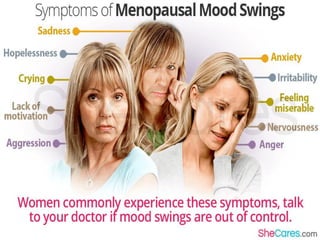
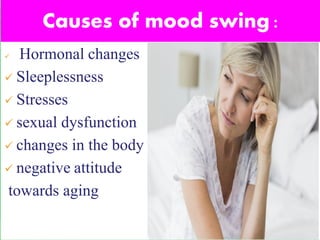
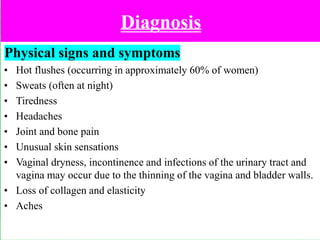
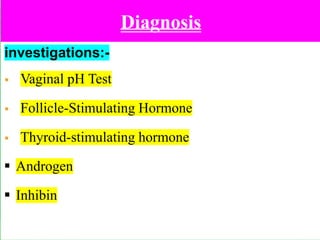
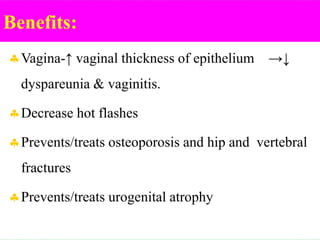
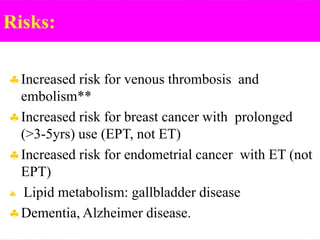
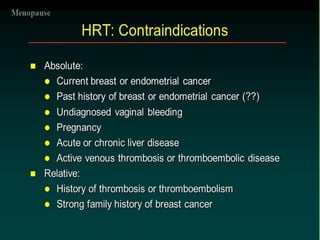
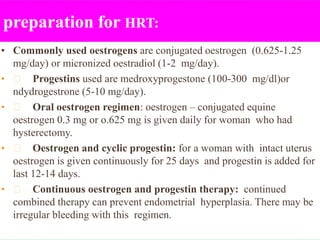
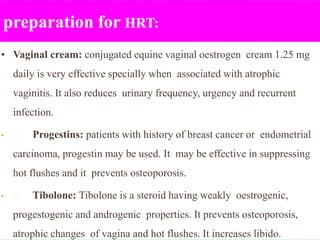
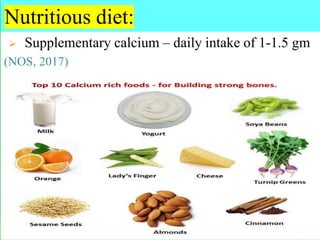
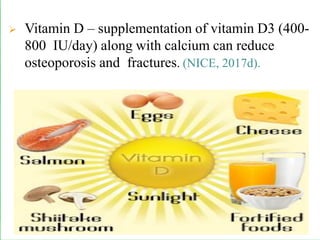
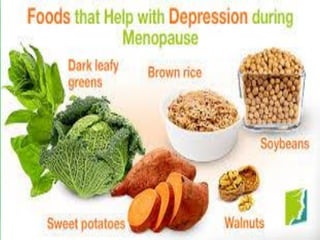
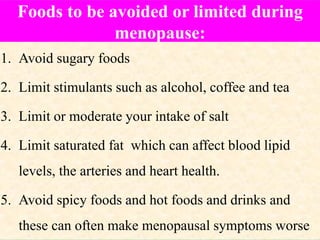
The document provides a comprehensive overview of menopause, highlighting its definition, physiological changes, symptoms, and management strategies. It discusses the hormonal, psychological, and physical impacts of menopause on women's health, including risks such as osteoporosis and heart disease, along with tips for lifestyle modifications and hormonal treatment options. Additionally, it outlines the role of healthcare providers in supporting women through menopause, emphasizing personalized approaches to care.