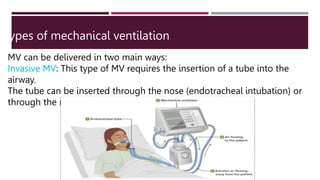
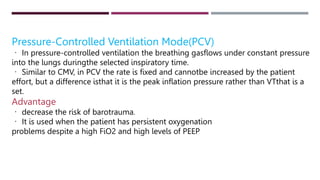
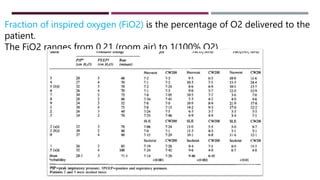
The document provides a comprehensive overview of mechanical ventilation, including definitions, indications, types, modes, and parameters, as well as potential complications and weaning processes. It details nursing care responsibilities, the importance of monitoring and communication, and best practice bundles to prevent complications such as ventilator-associated pneumonia. Specific criteria for weaning patients off mechanical ventilation and various methods for doing so are also discussed.