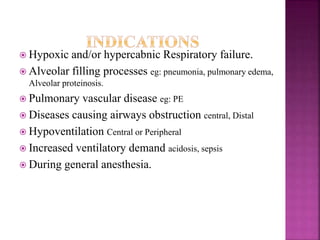
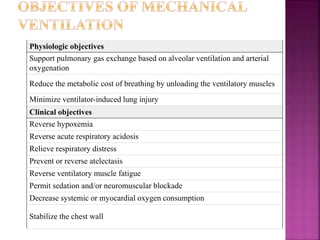
1. The document discusses mechanical ventilation, including its history, principles, objectives, modes, settings, complications, and clinical applications.
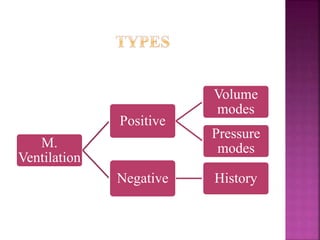
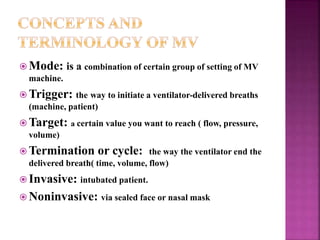
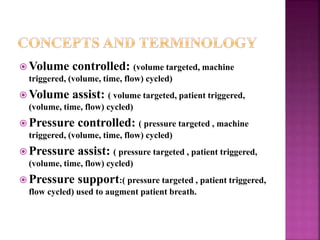
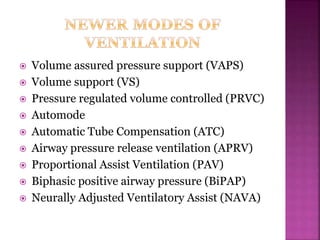
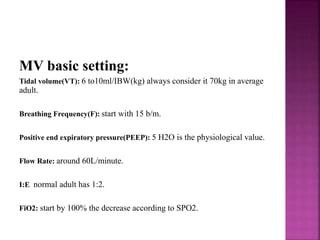
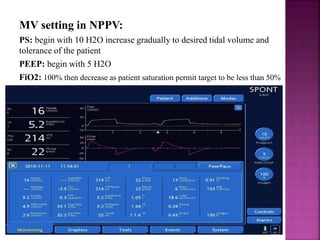
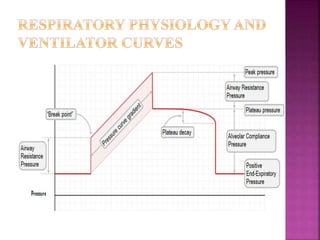
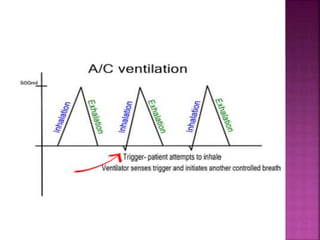
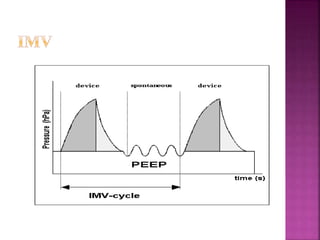
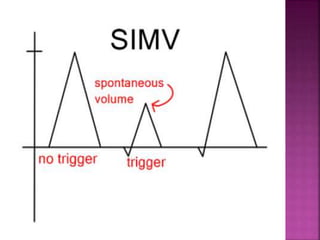
2. Key points include the various modes of mechanical ventilation like volume controlled, pressure controlled and pressure support. It also outlines objectives, settings, and safety principles of mechanical ventilation.
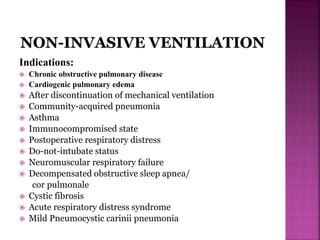
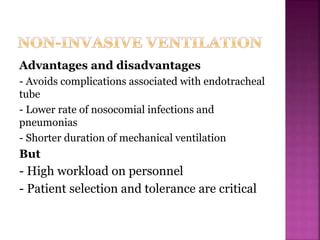
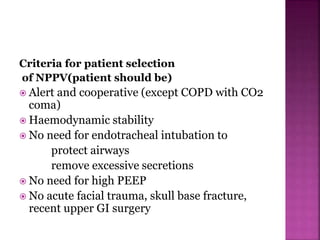
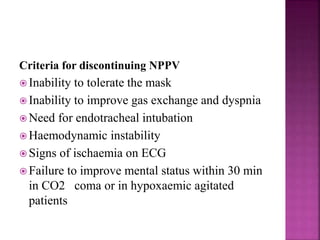
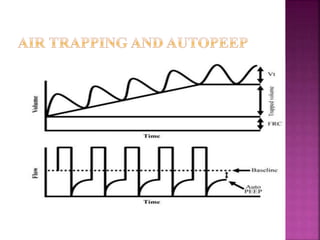
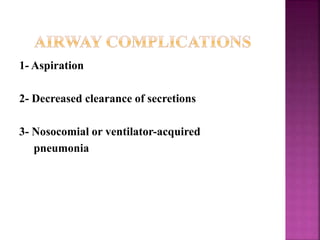
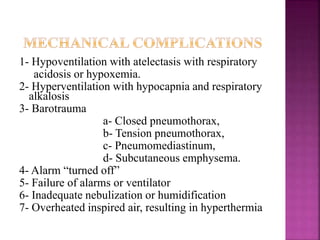
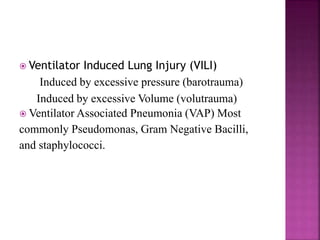
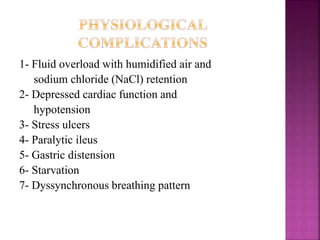
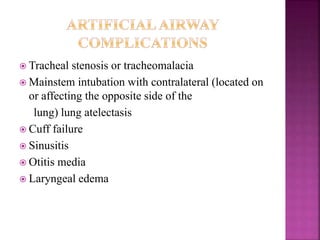
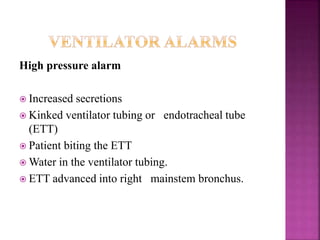
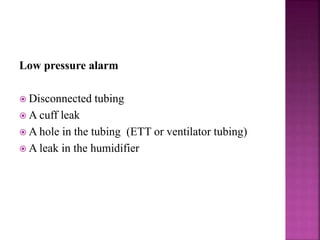
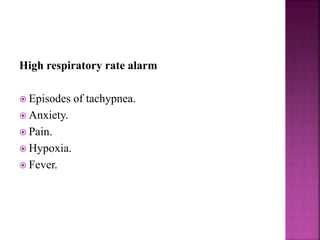
3. Complications discussed are ventilator-induced lung injury, ventilator-associated pneumonia, and physiological and artificial airway complications. Clinical applications include indications, contraindications and criteria for use of non-invasive positive pressure ventilation.