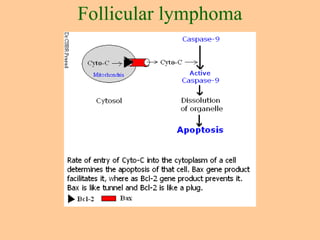
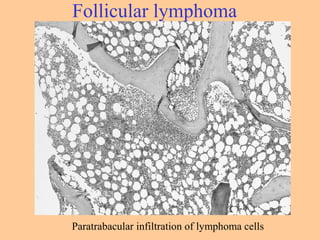
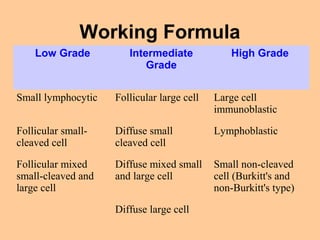
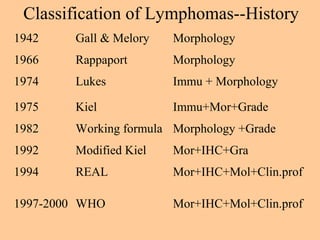
This document discusses techniques used to study lymphomas, including immunophenotyping, cytogenetics, and molecular analysis. Immunophenotyping helps differentiate benign from malignant processes and B and T cell neoplasms by identifying cell surface markers. Cytogenetics identifies chromosomal translocations which are characteristic of different lymphomas. Molecular analysis finds Ig and TCR gene rearrangements in B and T cell malignancies. The document also summarizes different classifications of lymphomas and characteristics of specific lymphoma types like CLL/SLL, follicular lymphoma, DLBCL, and Burkitt's lymphoma.
























![•T-cell and putative NK-cell neoplasms
•Precursor T-cell neoplasms
•Precursor T-cell acute lymphoblastic leukemia (T-ALL)
•Lymphoblastic lymphoma
•Peripheral T-cell and NK-cell neoplasms
•T-cell CLL/prolymphocytic lymphoma
•T-cell granular lymphocytic leukemia
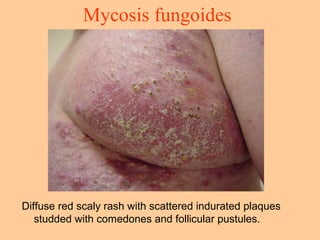
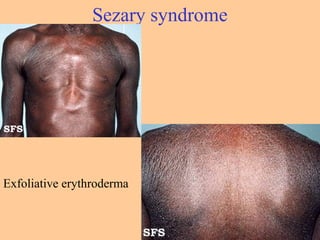
•Mycosis fungoides/Sézary syndrome
•Peripheral T-cell lymphoma, not otherwise characterized
•Hepatosplenic gamma/delta T-cell lymphoma
•Subcutaneous panniculitislike T-cell lymphoma
•Angioimmunoblastic T-cell lymphoma
•Extranodal T-cell/NK-cell lymphoma, nasal type
•Enteropathy-type intestinal T-cell lymphoma
•Adult T-cell lymphoma/leukemia (with human T-cell leukemia virus type 1 [HTLV-1])
•Anaplastic large cell lymphoma, primary systemic type
•Anaplastic large cell lymphoma, primary cutaneous type
•Aggressive NK-cell leukemia
WHO classification of lymphomas](https://image.slidesharecdn.com/lymphomas-1-nhl-151030055335-lva1-app6891/85/Lymphomas-1-nhl-28-320.jpg)