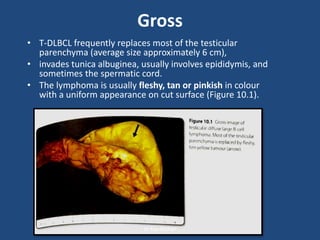
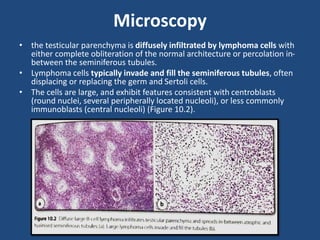
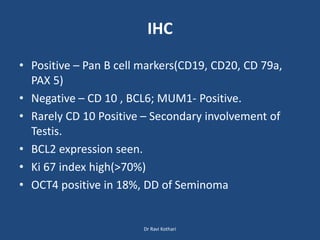
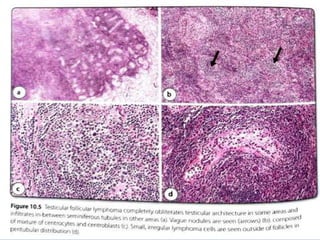
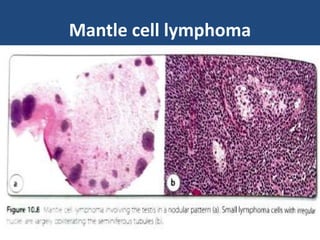
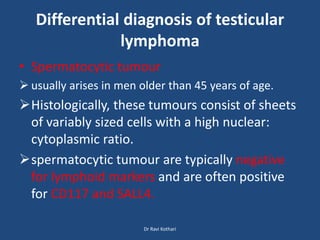
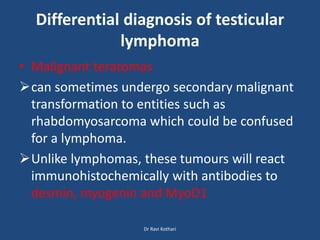
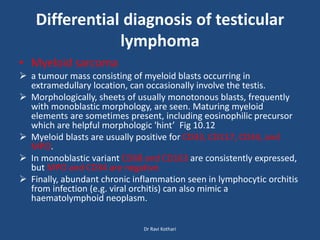
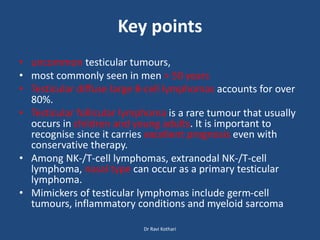
Lymphoma involving the testis is uncommon, accounting for 1-2% of testicular tumors. The most common type is diffuse large B-cell lymphoma (DLBCL), which accounts for 80-90% of cases and typically affects older men with a mean age of 60 years. Testicular follicular lymphoma is rare but usually occurs in children and young adults, carrying an excellent prognosis even with conservative therapy. Other types include Burkitt lymphoma, B-cell lymphoblastic leukemia/lymphoma, and rarely NK/T-cell lymphoma or plasma cell neoplasms. Differential diagnoses that can mimic lymphoma include seminoma, spermatocytic tumor, malignant teratomas, and myeloid sarcoma