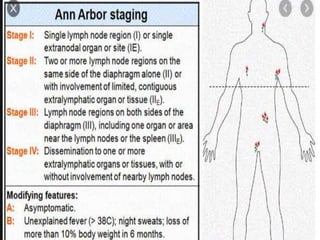
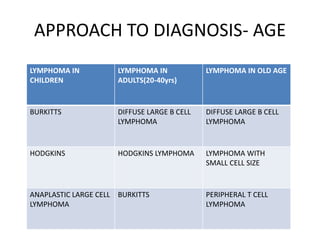
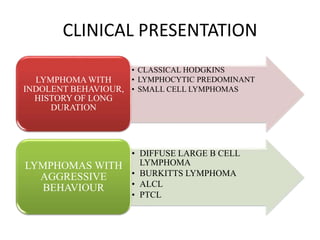
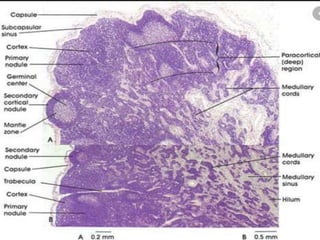
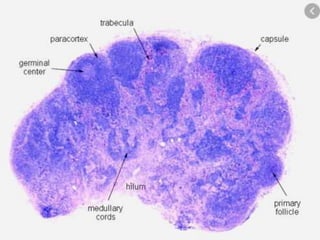
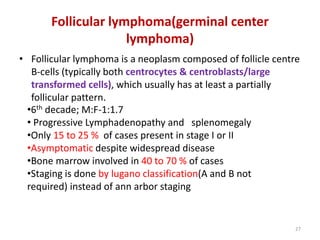
- A 55-year-old male presented with peripheral and central lymphadenopathy and splenomegaly but was asymptomatic. A lymph node biopsy was performed.
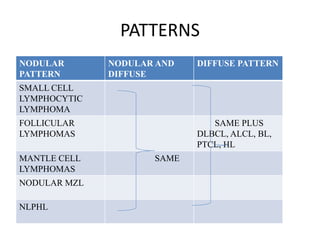
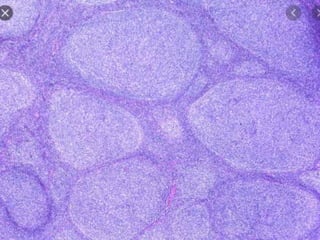
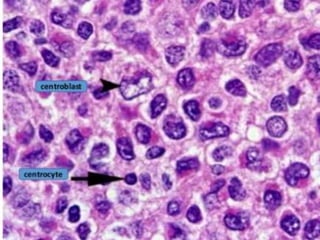
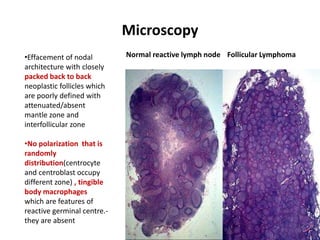
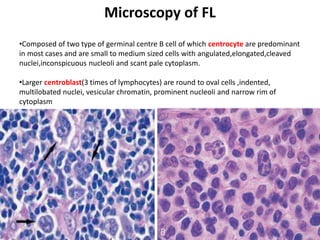
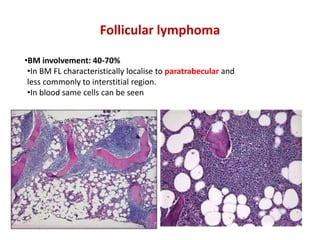
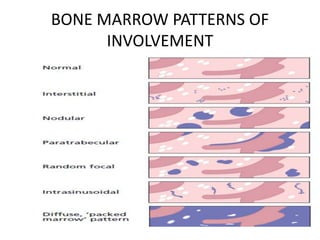
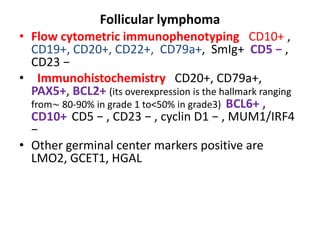
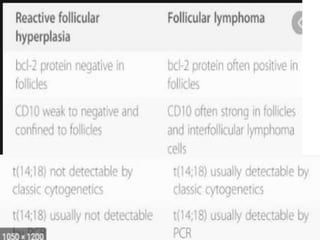
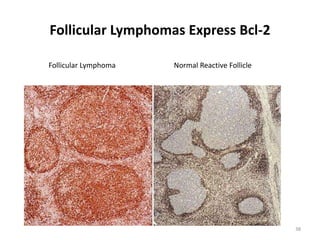
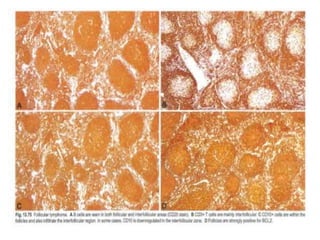
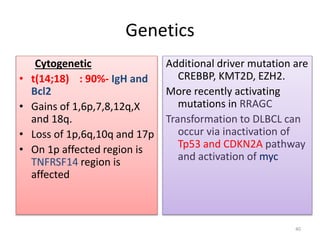
- Microscopic examination revealed features consistent with follicular lymphoma (FL), a neoplasm composed of follicle center B-cells which usually has at least a partially follicular pattern. FL is characterized by t(14;18) translocation and involves bone marrow in 40-70% of cases.
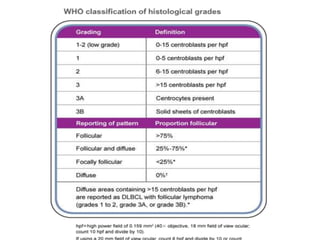
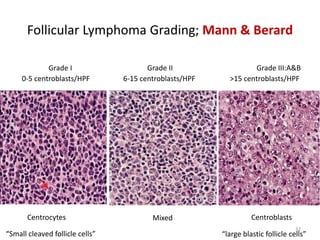
- FL was further classified based on the number of centroblasts per high power field according to the Mann and Berard grading system into Grade I (0-5 centroblasts/HPF), Grade II (6-15 centroblasts/