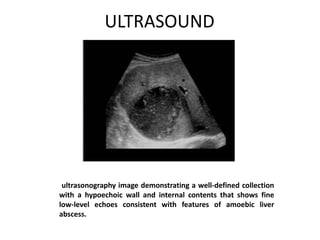
Liver abscesses occur when bacteria, protozoa, or fungi infect and destroy hepatic tissue. There are two main types: pyogenic (caused by bacteria) and amebic (caused by the protozoan Entamoeba histolytica). Common symptoms include fever, right upper quadrant pain, and hepatomegaly. Imaging tests like ultrasound and CT are used to detect abscesses. Treatment involves antibiotics, drainage of large abscesses, and treating any underlying infection. Outcomes are generally good but complications can include sepsis, empyema, and rupture.